The fluid pressure inside the eye, known as intraocular pressure (IOP), is an important metric for evaluating a person's risk of glaucoma. There are currently two different ways to measure IOP, both of which require a trip to the ophthalmologist. A prototype sensor developed by engineers at the University of Washington (UW) is designed to be placed permanently in a person's eye to track changes in eye pressure and more effectively manage the disease.
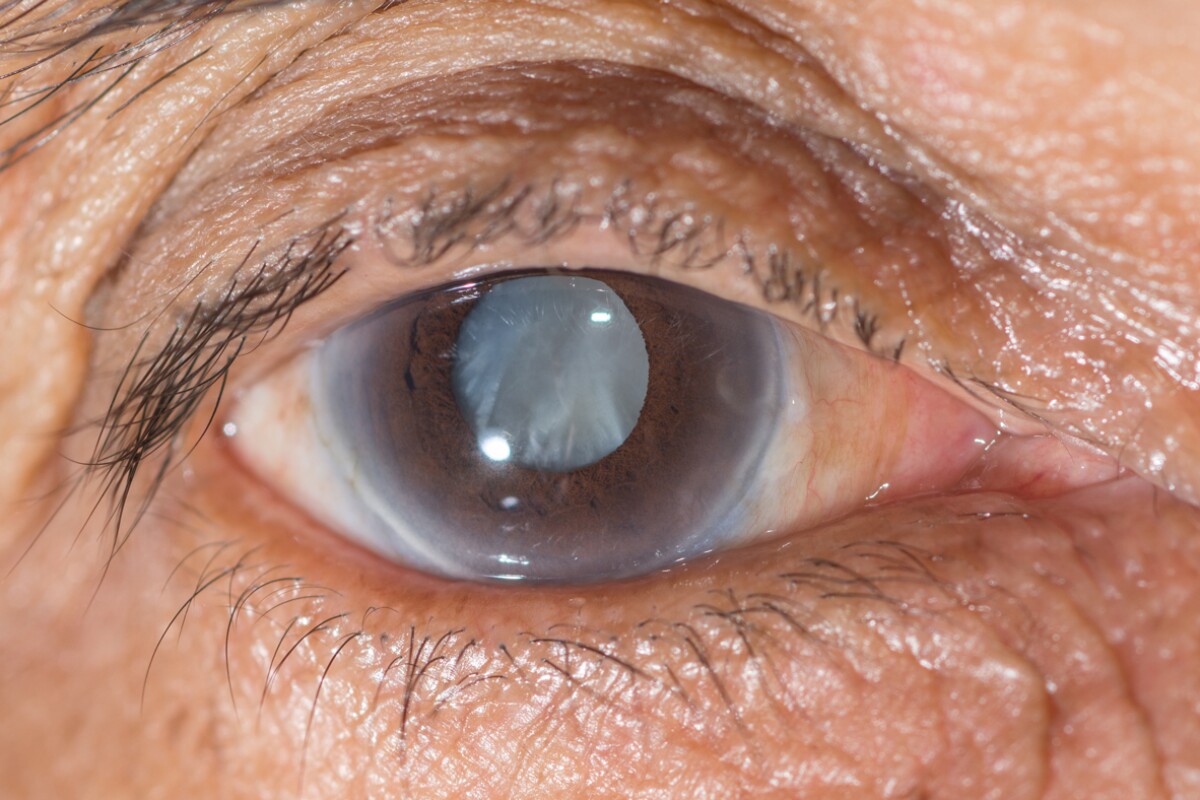
Glaucoma is a group of eye disorders usually associated with high eye pressure that cause damage to the optic nerve and can result in blindness. Although patients at risk of the disease may have their eye pressure checked several times a year, but with eye pressure thought to change throughout the day, this may still not be enough to detect the early warning signs and provide treatment when it is most effective.
"Oftentimes damage to vision is noticed late in the game, and we can’t treat patients effectively by the time they are diagnosed with glaucoma," says Yi-Chun Shih, a former doctoral student at UW. "Or, if medications are given, there’s no consistent way to check their effectiveness."
With the goal of developing an easy way to monitor eye pressure for management of glaucoma, engineers at UW have developed a prototype device that is designed to be embedded with an artificial lens during cataract surgery. The team says that implanting the device during such surgery makes sense because both glaucoma and cataracts affect a similar demographic. Cataract surgery is also a common procedure carried out on millions of people annually, so implanting the sensor at the same time would save patients from a second surgery while making their replacement lens "smarter" and more functional.

The low-power sensor uses radio waves for wireless power that is harnessed via a thin antenna that circles its perimeter, roughly tracing a person's iris. This powers a small pressure sensor chip that detects any shifts in frequency that can signify a change in eye pressure, sending the data to a nearby receiver, which could take the form of a dedicated handheld device or possibly be built into a smartphone. The receiver would be responsible for calculating the actual eye pressure and tracking and recording any changes in real-time.
"No one has ever put electronics inside the lens of the eye, so this is a little more radical," said Karl Böhringer, a UW professor of electrical engineering and of bioengineering. "We have shown this is possible in principle. If you can fit this sensor device into an intraocular lens implant during cataract surgery, it won’t require any further surgery for patients."
The team says it has already tested the prototype sensor by embedding it in the same flexible silicon material used to create artificial lenses in cataract surgeries. While the current prototype is still too large to fit into an artificial lens, the UW team is confident it will be possible to downscale the device to the required size. It is now focused on this task, with the ultimate goal of designing a device that is affordable for patients.
The UW team has published the results of their study in the Journal of Micromechanics and Microengineering. They have also filed patents on an initial prototype of the device.
Source: University of Washington