Hijacking sperm cells to create little robots might seem far out, but that's exactly what researchers from the Dresden Institute for Integrative Nanosciences have done. Their "spermbots" consist of live sperm cells in little tubes, that can be magnetically controlled to move in a desired direction until they reach their destination and do their job – they're currently robust enough to even guide a specific sperm cell to an egg cell. The scientists hope that further development will allow the technology to offer a viable alternative to parents trying to have a child through in-vitro fertilization. When perfected, the spermbots could also be used as a safe means for drug delivery and gene manipulation.
One of the major challenges in creating micro robots that can potentially travel within the human body is the issue of a safe fuel source. Nanobots with engines efficient enough to propel themselves through bodily fluids need to carry fuel that's often toxic to the human body, and sometimes these machines can pass through into the cells and affect their functioning. To overcome these problems, the Dresden team began looking at safer alternatives to artificial nano engines.
"We thought of using a powerful biological motor to do the job instead and we came up with the flagella of a sperm cell, which is physiologically less problematic," Professor Oliver G. Schmidt, the Institute's Director, tells Gizmag. "The idea came to us five years ago when I noticed that sperm cells are of similar size to microtubes we can fabricate."
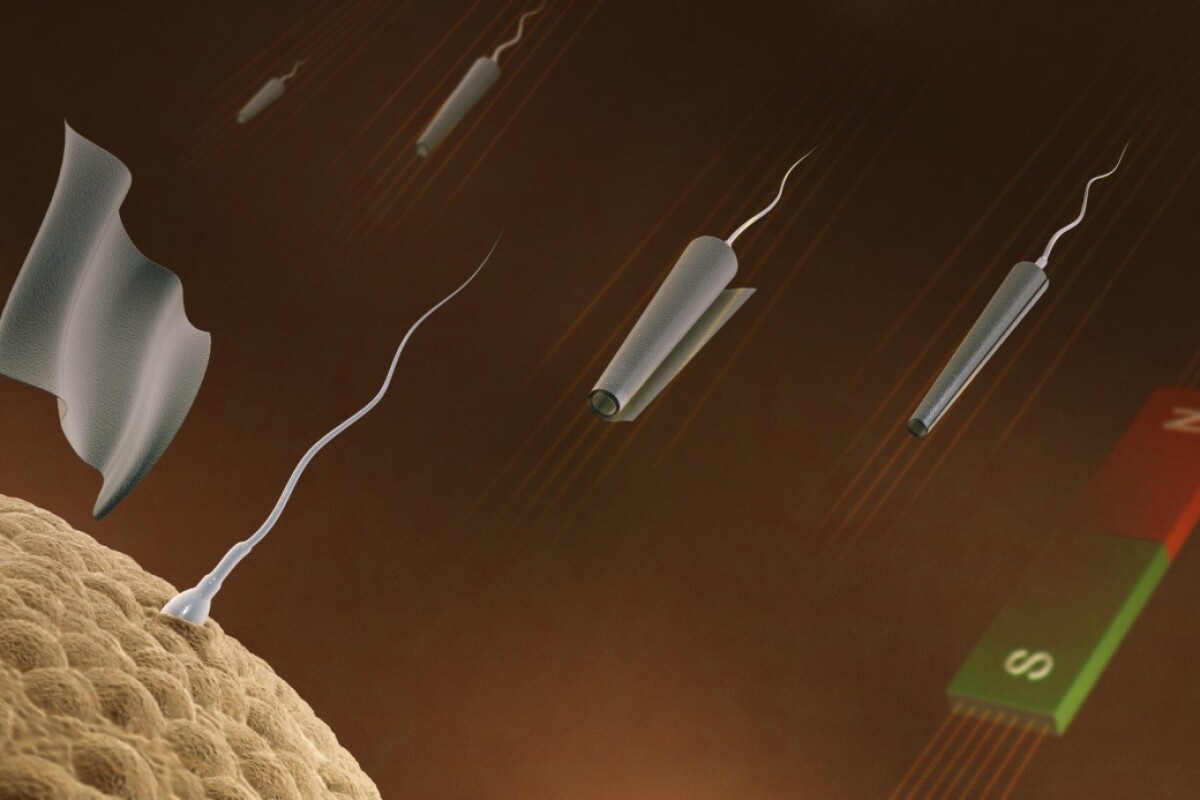
To create biorobots out of sperm cells, the researchers began working with bovine (bull) sperm cells – which are similar in size to human sperm cells. The first step was to create thin conical magnetic tubes capable of trapping sperm cells out of a titanium and iron film. The microtubes are rolled up in a way that makes one end larger than the other, with a diameter that's slightly larger than that of a bull sperm head.
When live sperm cells are added to a solution containing these microtubes in a petri dish, the sperm swim about and enter the tubes randomly. Once inside, they are locked down mechanically and begin pushing the tube forward as they move about. Magnetic material present in the tubes makes it possible to get remote-controlled sperm.

"We used a magnetic field to guide the direction of the so-called 'spermbots' and changed the temperature to control their speeds," Schmidt explains. "All this was done in-vitro, i.e. outside the body."
Once the spermbot reaches the desired location, it could be manipulated magnetically to release the sperm. While the researchers are still working on the issue, they state that it should be possible to set the sperms free by altering the temperature to unroll the tubes, just before they reach the egg. The microtubes could be removed from the body by applying the magnetic field appropriately, with little if any risk.
"Compared to magnetic nanoparticles, magnetic microtubes are not as hazardous, because they do not enter the cells," Veronika Magdanz, a researcher at the Institute tells us. "They are larger than the cell itself."
Sperm cells are ideal candidates to transform into biobots since they are easily available, harmless and efficient at swimming through bodily fluids. With a chip about 22 x 22 mm (0.8 in x 0.8 in) in size, the researchers have been able to produce around 200,000 well-defined microtubes. In initial tests, the team worked with thawed-out bull sperm cells that remained viable for a few hours.
It's possible to make hundreds of spermbots with microtubes obtained from a single chip, each capable of traveling up to 100 micrometers per second. That's about two body lengths of the sperm-driven tube per second – comparable to a 1.80 m (6 ft) tall human swimming the 50 m (160 ft) free-style in 14 seconds.
The team plans to try assisted fertilization with animals before starting experiments and clinical trials with human sperm. Since it's possible to control the path of these spermbots to the tune of a few micrometers, the spermbots could ultimately also be utilized to ferry drugs and payloads anywhere within the body.
A paper describing the technology, entitled "3D Magnetic Control Of Microjets" is due to be published soon in the journal Applied Physics Letters.
Source: IFW Dresden