According to theInternational Diabetes Federation, 387 million people around the world sufferfrom diabetes, with this number expected to rise to 592 million by 2035. Thatadds up to a lot of blood sugar checks, diet watching and insulin shots, butresearchers in the US have developed a patch that could revolutionize how the disease is managed. The patch contains of more than 100microneedles, each automatically secreting insulin into the bloodstream whenrequired.
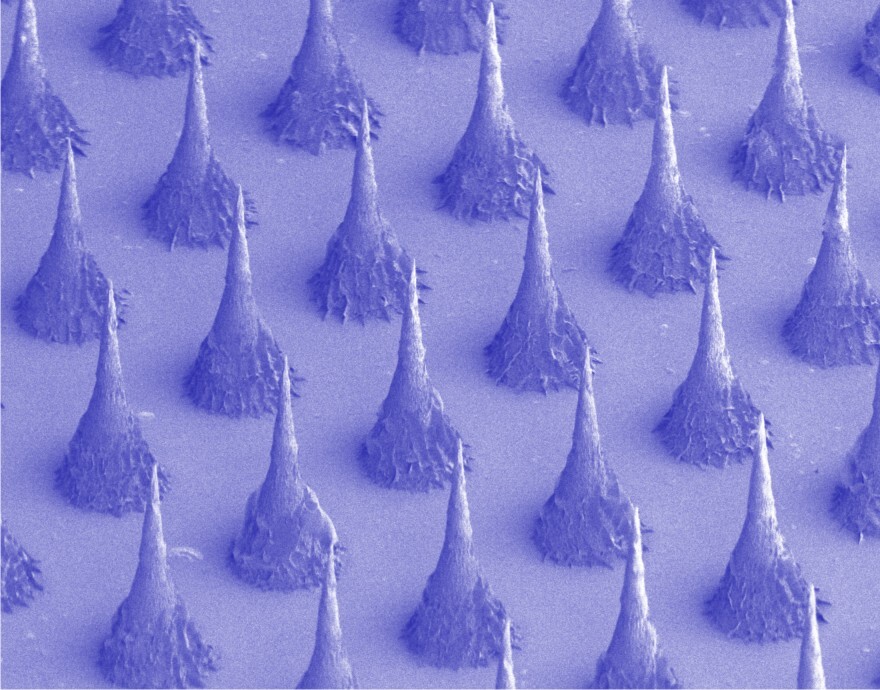
The thought of over ahundred microneedles replacing a single needle might not sound like an appealing trade, but their tiny size makes them less painful than a standard needle despite their numbers. Each microneedle is about the size of an eyelash, with more than 100crammed onto a patch no bigger than a penny.
Indeveloping the patch, researchers at the University of North Carolina (UNC) andNorth Carolina State University (NC State) sought to mimic the body's betacells, which both produce and store insulin in tiny sacs called vesicles, aswell as signalling the release of insulin into the bloodstream when they detectan increase in blood sugar levels.
To create artificialvesicles, the team started with hyaluronic acid (HA), which is a naturalsubstance used in many cosmetics. They then combined HA with 2-nitroimidazole(NI), an organic compound commonly used in diagnostics, to produce a newmolecule that was hydrophilic (has an affinity for water) at one end andhydrophobic (repels water) at the other. Similar to the way oil dropletscoalesce in water, a mix of these new molecules self-assembled into a vesiclewith the hydrophobic ends pointing inwards and the hydrophilic ends pointingoutwards.
Into each of thesevesicle structures, which were 100 times smaller than the width of a humanhair, the researchers inserted a core of solid insulin and glucose-sensingenzymes. Lab experiments showed that in response to a rise in blood sugarlevels, excess glucose flooded into the artificial vesicles and was convertedinto gluconic acid by the enzymes. This process consumed oxygen, the resultinglack of which turned the hydrophobic NI molecules hydrophilic and prompted thevesicles to fall apart and release their insulin payload.
Once they had createdthese "intelligent insulin nanoparticles," the researchers needed adelivery method, deciding upon incorporating the artificial vesicles into anarray of microneedles. These were created using a more rigid form of the samehyaluronic acid that went into the nanoparticles, thereby enabling the microneedles topierce the skin. These were than placed on a thin silicon strip to form a patchwith an array of over 100 microneedles, which are able to penetratethe skin and deliver their payload into the capillaries just below the surface.
In tests, one group ofmice with type 1 diabetes was given a standard insulin injection, which causedtheir blood sugar levels to drop back to normal before quickly climbing backinto the hyperglycemic range. However, the blood glucose levels of another groupof mice dropped to normal levels within 30 minutes of being treated with themicroneedle patch, and stayed that way for several hours. The researchers believe the blood sugar-stabilizing effects of the patch could last even longer in humans, as mice are less sensitive to insulin than we are.
By varying the amount ofglucose-sensing enzymes in the vesicles, the researchers also found they wereable to tune the patch so it altered blood glucose levels only within a certainrange. Additionally, the patch didn't send blood sugar levels plummeting todangerously low levels, which can be a hazard with administering standardinjections too frequently.
"We have designed apatch for diabetes that works fast, is easy to use, and is made from nontoxic,biocompatible materials," says co-senior author Zhen Gu, PhD, a professorin the Joint UNC/NC State Department of Biomedical Engineering. "The wholesystem can be personalized to account for a diabetic’s weight and sensitivityto insulin, so we could make the smart patch even smarter."
The team'sultimate goal is to develop a patch that would only need to be changed everyfew days – which would surely be an attractive proposition for diabetics.
Their study appearsin the Proceedings of the National Academy of Sciences.
Source: University ofNorth Carolina