A team of scientists from the University of Illinois at Chicago and Queensland University of Technology in Australia has demonstrated a new, cheap and fast device that can detect floating cancer cells in a tiny blood sample.
There are a variety of different methods currently being investigatedin the hope of developing accurate blood tests to detect cancer.From tracking cancerous RNA traces, to detecting a unique DNA nanostructure common to almost all cancer types, we are undeniably onthe cusp of an exciting new wave of diagnostics.
Perhaps one of the more straightforward prospective cancer bloodtests being investigated is detecting circulating tumor cells (CTCs).These are cells that shed off the primary tumor into a person'sbloodstream but the big challenge scientists have faced is producinga device that can detect these single cells, often only present inextraordinarily small quantities.
"A 7.5-milliliter tube of blood, which is a typical volume for ablood draw, might have ten cancer cells and 35-40 billion bloodcells," explains Ian Papautsky, a corresponding author on the newresearch. "So we are really looking for a needle in a haystack."
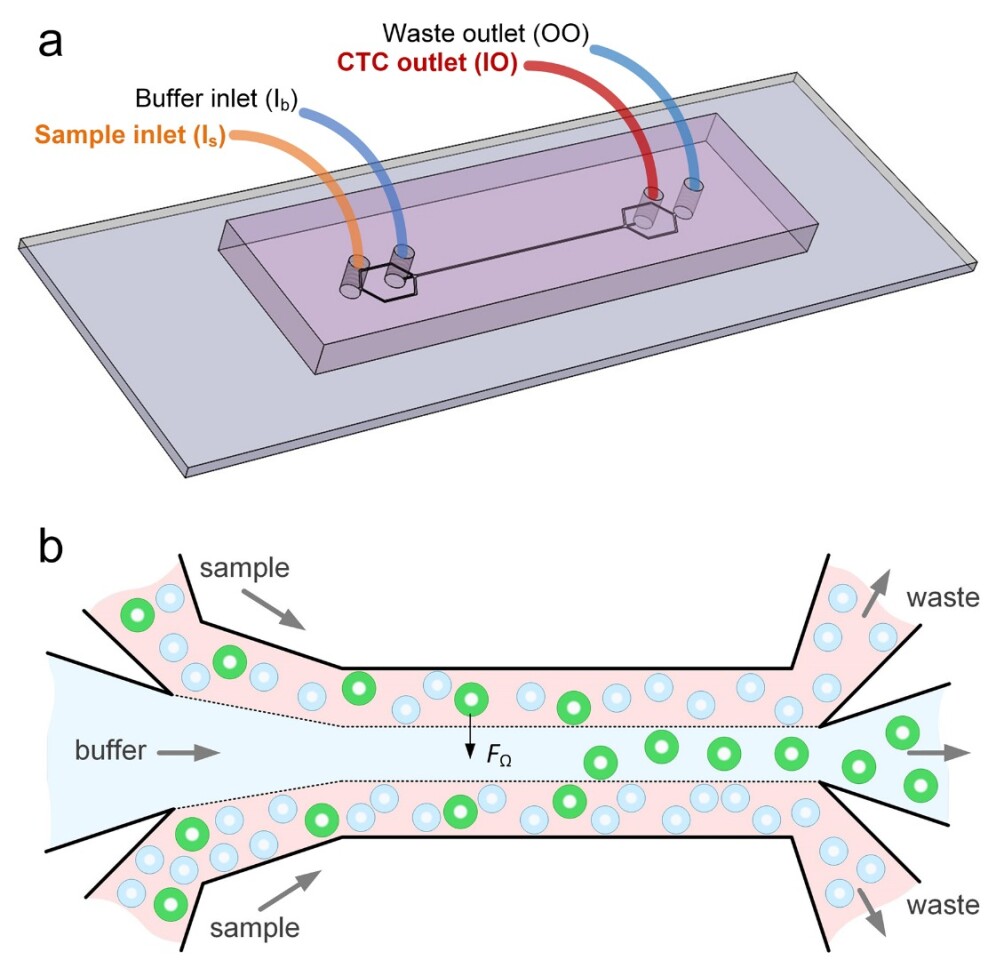
The newly developed diagnostic device utilizes microfluidic technology toseparate cancer cells from other cells in any given blood sample.Unlike other microfluidic devices that use certain biomarkers to latch onto tumor cells within a sample, often called affinity separation, the new device harnesses thetheory of size-dependent inertial migration. Essentiallythe device filters out the CTCs based on the cells unique sizecompared to other elements found in a blood sample.
"Using size differences to separate cell types within a fluid ismuch easier than affinity separation which uses 'sticky' tagsthat capture the right cell type as it goes by," says Papautsky."Affinity separation also requires a lot of advanced purificationwork which size separation techniques don't need."
The results from early testing are nothing short of remarkable.The experimental device successfully captured 93 percent of cancercells from a 5 ml blood sample spiked with 50 CTCs. A further, evenmore difficult test, spiking a 5 ml sample with just 10 cells returnedan 83 percent detection rate. Testing the device on blood samplesfrom eight cancer patients, the method identified CTCs in all but twoof the samples, with the researchers suggesting the error rate wassimply due to only testing very small volumes of blood.
These first tests of the device looked atnon-small-cell-lung-cancer CTCs but the researchers believe thesystem should be adaptable to a variety of other cancer types such asbreast and liver cancers. As long as the CTCs are larger than bloodcells the device should be broadly applicable, however theresearchers do note that a minimal volume of rare CTCs can be smallerthan blood cells and may be missed by the device.
The next step for the researchers is to further verify thedevice's efficacy in wider trials, while also improving its accuracyby adding extra biomarkers such as cancer DNA detection.
The new research was published in the journal Microsystems and Nanoengineering.





