November 8, 2006 A new and very promising Laser-Ultrasound-Nanotechnology combination that detects malignant breast tumors one-fifth the size found with conventional technology has attracted U.S. Federal funding totalling US$3.8 million. The new federal funding will support Phase II research into breast and prostate cancer detection using laser optoacoustic imaging technology developed by Fairway Medical Technologies.
The research funding includes authorization of two National Cancer Institute grants:
* A US$2.7 million Phase II grant from The National Institutes of Health-National Cancer Institute (NIH-NCI) to further develop the imaging technology in laboratory animal tests, and to explore its use in attacking cancer tumor cells.
* A US$1.1 million SBIR (Small Business Innovation Research) Phase II grant by the National Cancer Institute to develop a commercial medical imaging system for early detection of prostate cancer that is able to provide real time visualization of small prostate cancers and to guide prostate biopsy procedures.
The optoacoustic technology will be introduced as a real-time screening tool for breast cancer detection and diagnosis, an estimated US$5.9 billion market in North America, by Seno Medical Instruments of San Antonio, which has purchased the technology and entered into a long-term development agreement with Fairway. Seno will also provide development funding for the technology’s initial commercialization steps.
Breast Cancer Detection
The new $2.7 million nanotechnology grant should allow Fairway to prove that optoacoustic imaging can locate tumors tagged with gold nanorods bound to antibodies against breast cancer-specific receptors. This new NIH-NCI funding authorization follows successful conclusion of Phase I research to optimize the imaging system and fabricate prototype gold nanorods.
Over four years of research and pilot studies by scientists at Fairway and The University of Texas Medical Branch at Galveston (UTMB) indicates the system can detect breast cancer tumors potentially as small as 2 millimeters, five time smaller than most malignant breast tumors detected currently. If this is confirmed in Phase II tests with laboratory animals, it would mean that the proprietary system will make it possible to identify tumors that are easily curable and currently undetectable.
Phase II NIH Research
“The goal of the Phase II breast cancer research is to determine whether the optimized imaging system will enable in vivo imaging of early in situ breast tumors in animals with excellent sensitivity,” said Alexander A. Oraevsky, PhD, Fairway’s Vice President of R&D and the Principal Investigator. “If we can establish its capability to visualize tumors in mice down to 2 to 5 millimeters in diameter with high molecular specificity and insignificant nanoparticle accumulation in normal tissue, we believe this technology will be at the doorway to commercial development through clinical trials,” he added.
“Our research under this grant will go a long way toward determining whether the gold nanorods will be beneficial in tagging the tumors in reducing breast cancer mortality by providing sensitive, inexpensive, convenient and safe molecular-specific technology for cancer therapy,” said Fairway president Jim Meador.
Importance of Early Detection
“Because detection and follow-up in the early stages of breast cancer offers a much greater chance of survival, even small improvements in breast cancer diagnosis and treatment may save tens of thousands of lives every year,” Meador said. Nearly 600,000 new cases of breast cancer are diagnosed worldwide each year, about 216,000 in the U.S. where almost 40,000 deaths will result. More than 10% of all American women develop breast cancer during their lifetimes.
Small early tumors confined to the breast can be cured with close to 100% success. Improvement in the breast cancer survival rate today compared with that of 25 year ago is attributed mainly to the fact that today breast tumors are being detected earlier. However, only 25% of malignant breast tumors are detected at the stage when the tumor is 10 mm or less. Fairway believes the technology may help to detect tumors earlier, so that the percentage of tumors detected before they spread into the blood and lymph systems will increase, resulting in a greater survival rate.
Prostate Cancer Detection
The new prostate cancer grant follows work performed under a 2005 Phase I grant to define the technical requirements for and to develop a laboratory prototype for a transrectal probe containing both an optical illumination system and an array of wide-band ultrasonic transducers. The Phase II grant will include studies in the canine model of prostate cancer performed in collaboration with the University of Teas Medical Branch in Galveston, Texas.
“Prostate cancer strikes one in six men in America,” Meador noted. “It is a disease that is nearly 100 percent treatable, if its detection is early. Even small improvements in early detection can save thousands of lives,” he said.
According to the National Prostate Cancer Coalition, prostate cancer is diagnosed every two-and-a-quarter minutes with over 234,460 new cases expected in 2006. Although deaths from prostate cancer are down nearly 10 percent from 2005, an estimated 27,350 American men will lose their lives to prostate cancer in 2006.
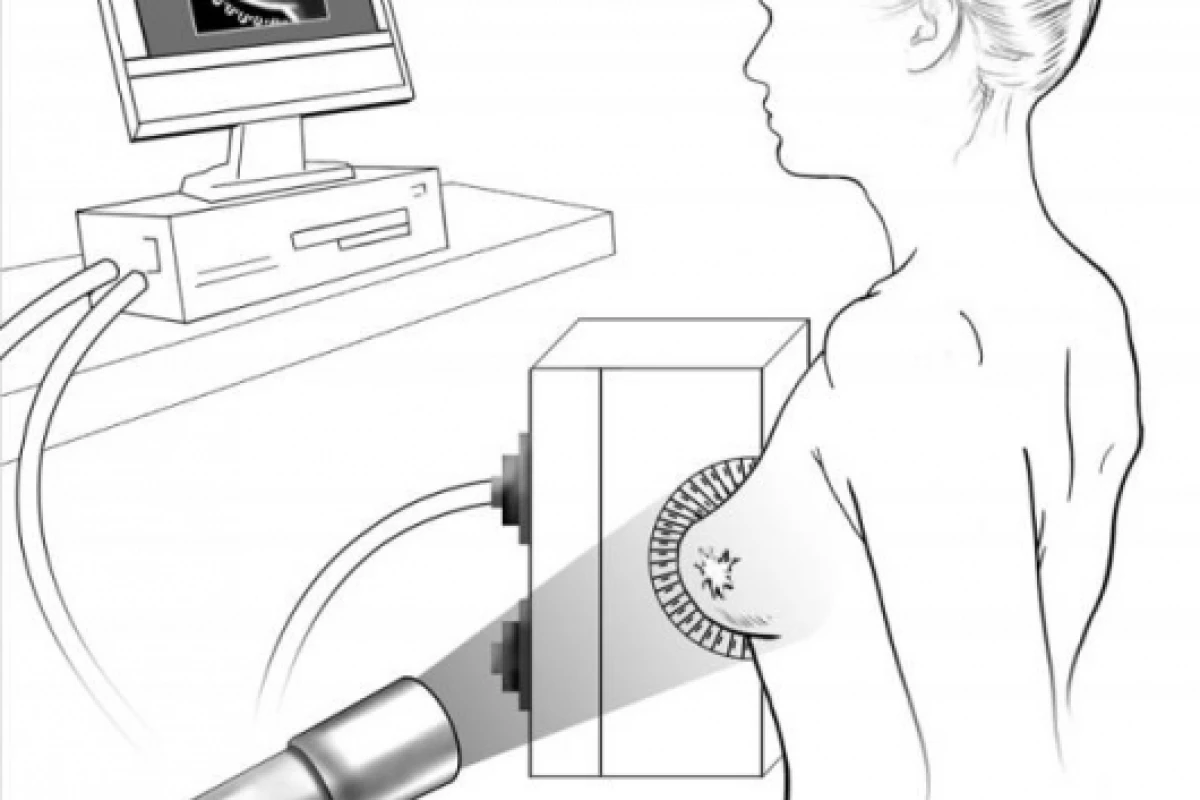
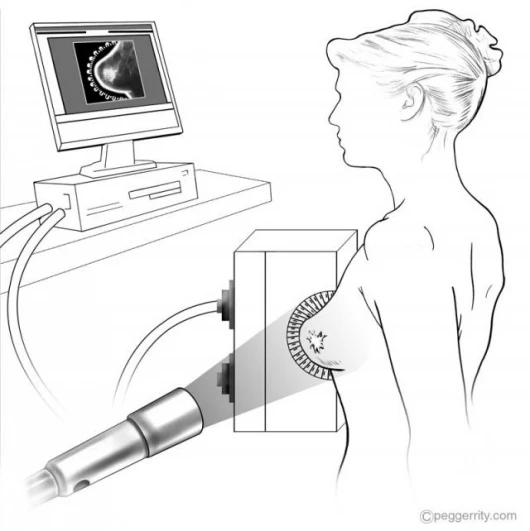
Hybrid Imaging Technology
The imaging system uses laser light to create contrast between normal and cancerous tissues, and laser-induced ultrasonic waves to carry diagnostic information. This hybrid technology is the only medical imaging technology with the potential to differentiate between malignant and benign tumors based on blood concentration and the oxygenation state of blood in the tumor, as well as to visualize them with high resolution (smaller than 1 mm) at tissue depths of up to 60 millimeters (~2.5 inches). Ongoing patient testing at UTMB under the direction of Tuenchit Khamapirad, M.D. has demonstrated the device’s capability to detect breast tumors in more than 20 patients.
Higher contrast and image definition is produced by using NOCA (Nanoparticulate Optoacoustic Contrast Agent) in combination with the imaging system. The NOCA technology binds gold nanorods -- with properties of optical absorption more than 1,000 times stronger than any organic molecule -- to antibodies against breast cancer-specific receptors, making it possible for the average cancerous tissue with only 10 nanorods per cell to become detectable relative to normal tissue. NOCA flows in the blood stream until it finds a specific molecule-receptor in the tumor; then it binds to the abnormal cells and, after being activated by laser light pulses of specific colors, sends a signal showing the location of the cancer. The nanoparticles may also contribute to the cancer cell’s death by becoming delivery vehicles for targeted anticancer drugs and for heat receptors for minimally invasive light-activated therapy.
Previous development work on optoacoustics and the imaging system has been funded by Fairway and by grants totaling over $3 million from the National Institutes of Health and the US Army’s Breast Cancer Research Program.
Privately held Fairway, which has more than doubled its manufacturing and research capacity in the past 24 months, develops and commercializes products based on proprietary or licensed technologies, and provides contract development and manufacturing services for outside clients. A portfolio company of BCM Technologies, the venture capital subsidiary of Baylor College of Medicine, Fairway has close relationships with most of the research institutions located in the Texas Medical Center, and has successfully orchestrated the design, development and manufacturing of scores of medical products, including FDA Class III (life supporting) devices.