Scientists have identified the first brainwave biomarkers for OCD, opening the door to personalized, on-demand brain stimulation that targets distressing compulsive behaviors as they arise.
Obsessive-compulsive disorder (OCD) is characterized by a pattern of unwanted thoughts and fears, known as obsessions, that lead to repetitive behaviors, or compulsions. These obsessions and compulsions interfere with daily activities and generally cause distress.
New research by the Netherlands Institute for Neuroscience and Amsterdam University Medical Center (Amsterdam UMC) has, for the first time, used implanted electrodes to identify deep brain activity patterns associated with obsessive thoughts and compulsive behaviors, which could serve as a biomarker for OCD. The discovery opens the door to more targeted treatment.
“In psychiatry, it is almost never possible to link a symptom so directly to brain activity,” said the study’s lead and co-corresponding author, Tara Arbab, PhD, a neuroscientist from Amsterdam UMC’s Department of Psychiatry and the Netherlands Institute for Neuroscience. “This study shows that it is possible. We’ve been doing this in animal models for years, but in patients, this technology is still new.”
For people with severe, treatment-resistant OCD, deep brain stimulation (DBS) is a promising treatment option. It involves surgically implanting thin electrodes deep within the brain to deliver electrical impulses to specific areas associated with the condition. DBS is meant to disrupt the abnormal neural circuits involved in OCD, potentially reducing the frequency of obsessive thoughts and compulsive behaviors.
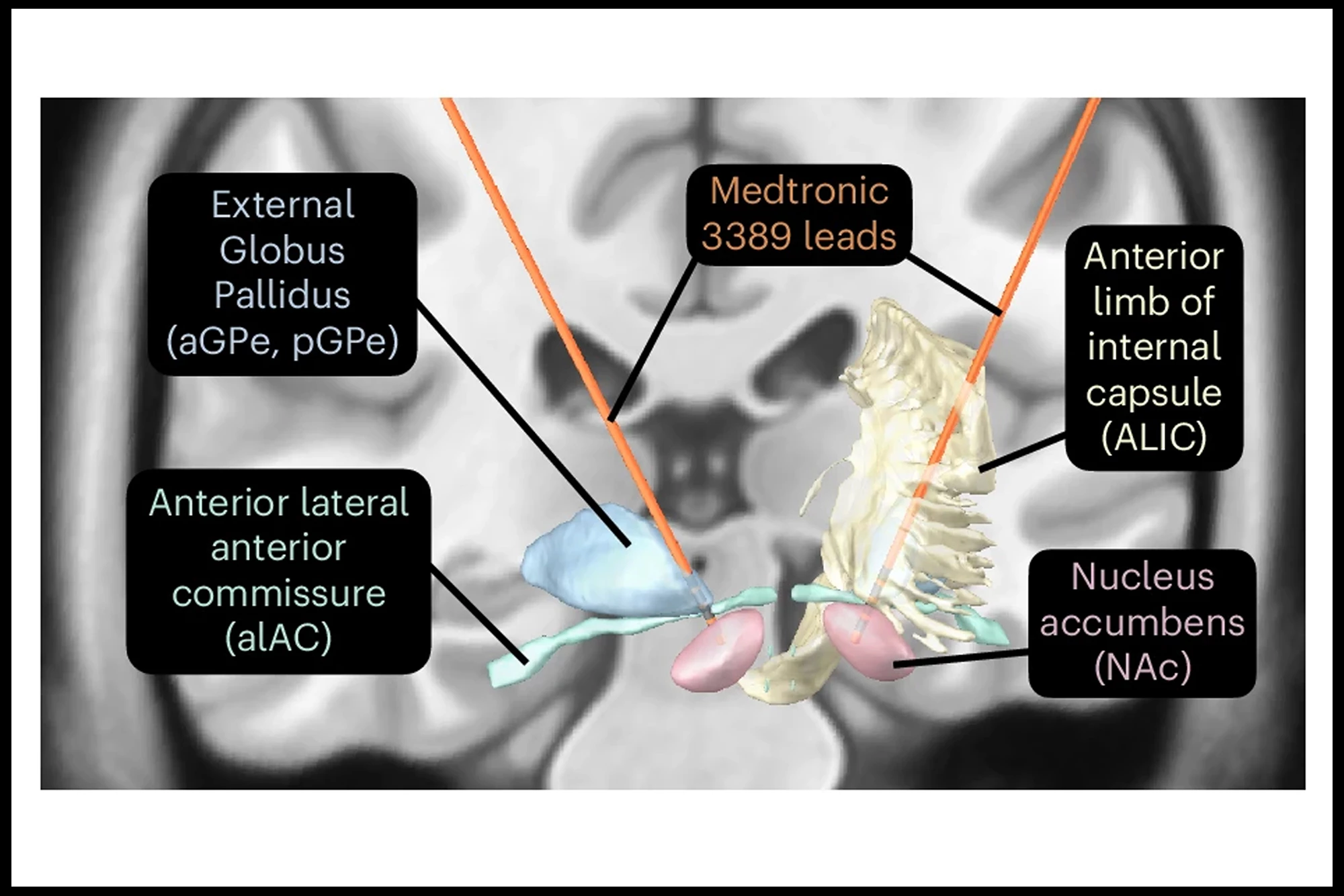
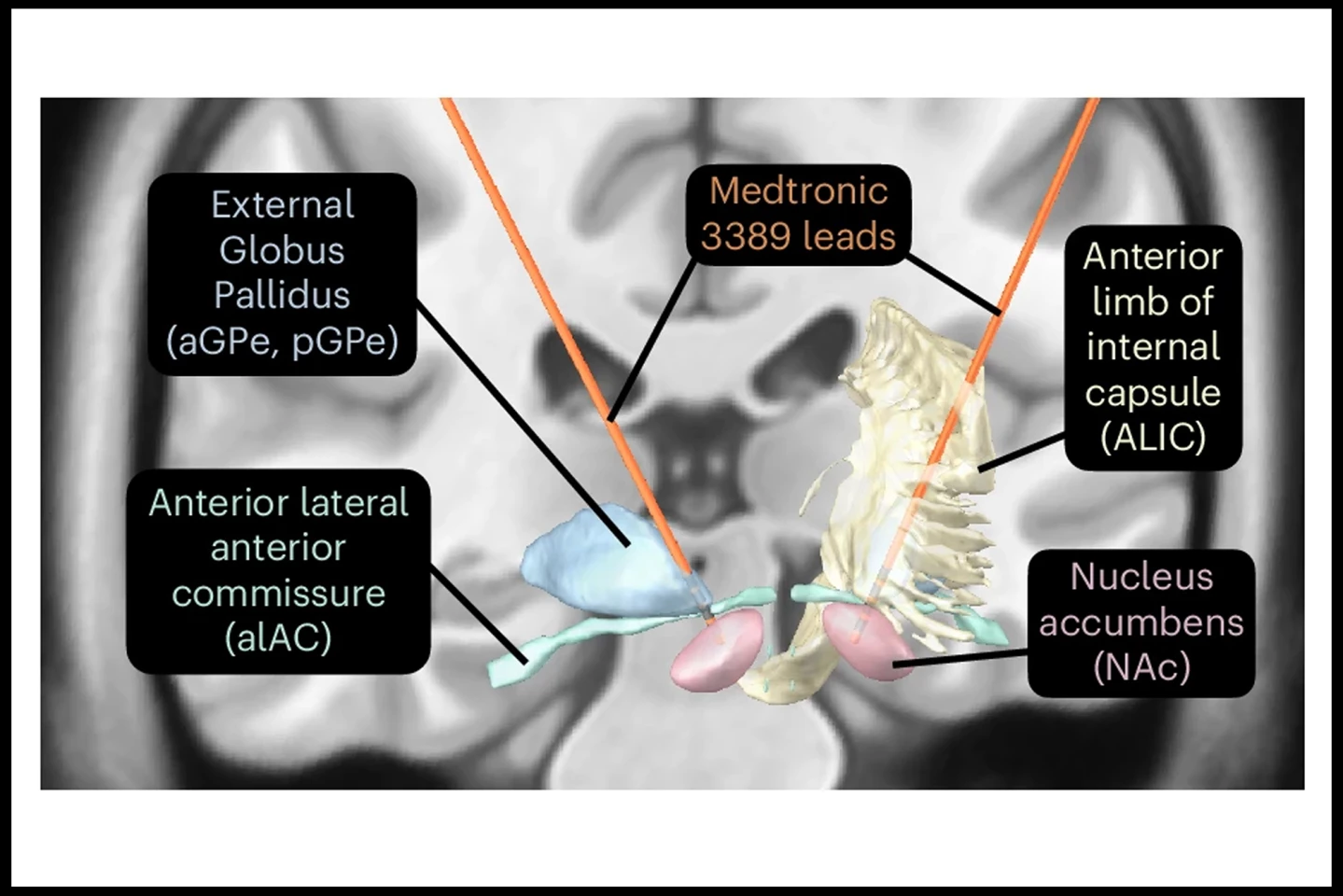
For the present study, the researchers implanted special DBS electrodes into the brains of 11 patients with treatment-resistant OCD. The electrodes could not only stimulate the brain but also record brain signals, specifically local field potentials (LFPs), which are brain waves linked to neuron activity. The researchers then provoked OCD symptoms in a controlled clinical setting.
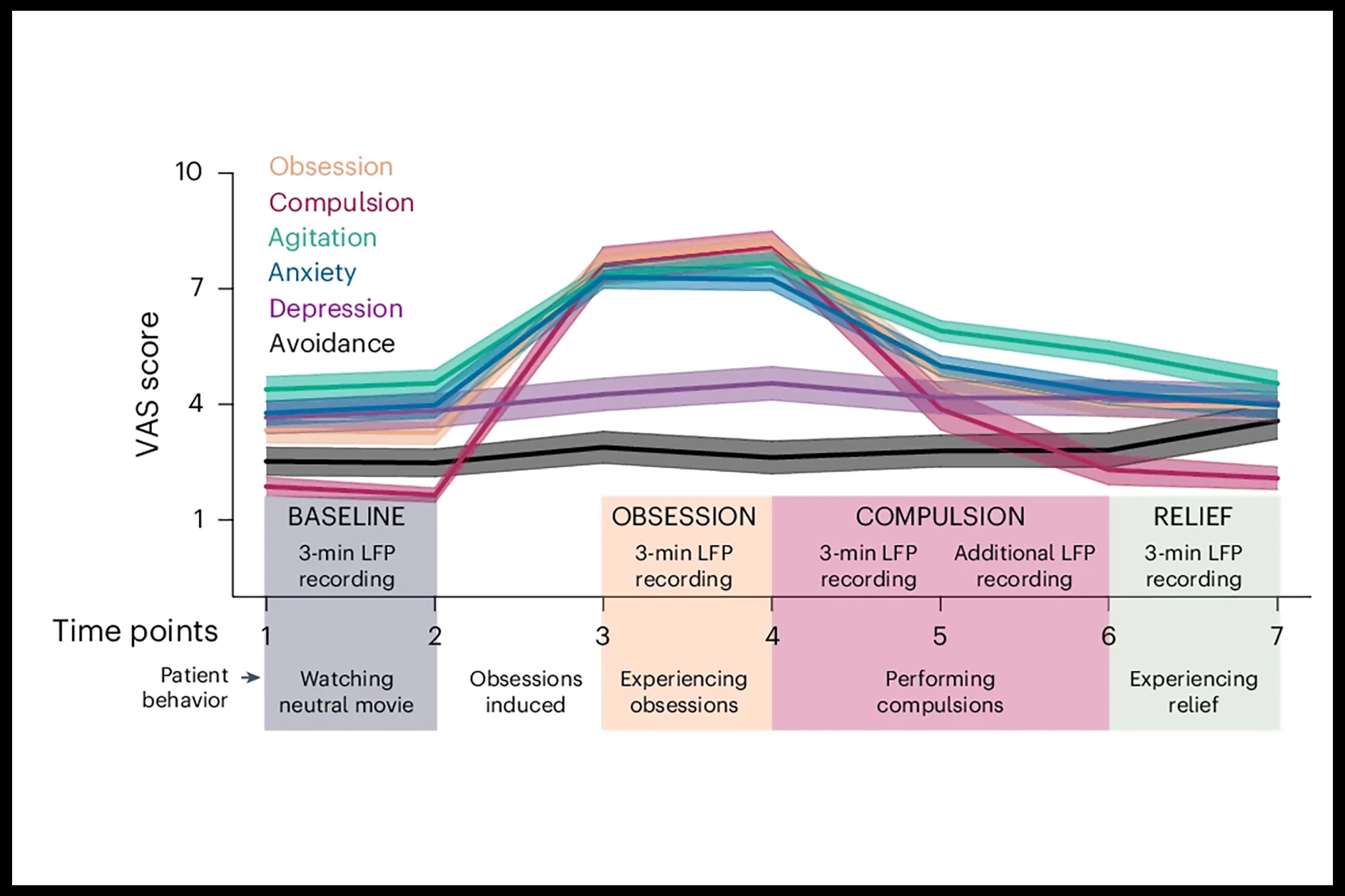
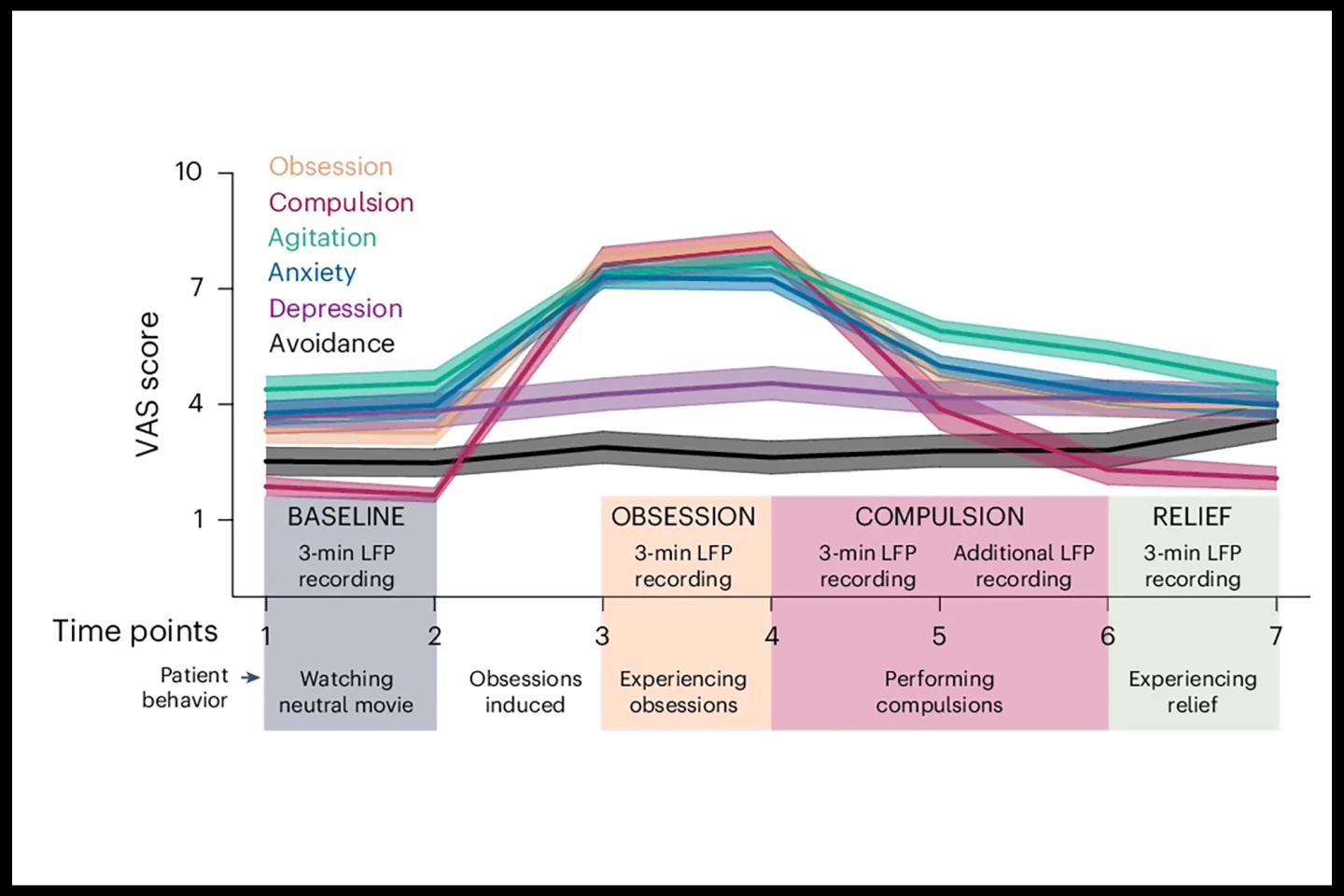
The patients watched a neutral video to start (baseline), then their personal obsession triggers were provoked. For example, if they had a fear of being infected or contaminated, which would normally drive compulsive hand-washing, they were asked to touch the floor. They were then allowed to engage in their compulsive behavior (e.g., hand washing) before finally sitting in relief after performing the compulsion.
During each of these four phases (baseline, obsession, compulsion, and relief), LFPs were recorded in three-minute intervals from the following specific areas involved in OCD:
- External globus pallidus (GPe). A key nucleus of the basal ganglia, the GPe is a group of structures involved in movement control and other functions. It’s a central processing hub, integrating inputs from various sources and sending outputs to influence motor and non-motor (e.g., reward processing, decision-making) pathways.
- Nucleus accumbens (NAc). A crucial part of the brain’s reward system, playing a role in motivation, pleasure, and addiction. It helps us associate actions with positive outcomes and also influences how emotional responses are translated into actions.
- Anterior limb of the internal capsule (ALIC). The ALIC connects the prefrontal cortex to other brain regions and acts as a pathway for fibers connecting the prefrontal cortex to deeper brain structures involved in emotion, cognition, and motivation.
- Anterior lateral anterior commissure (alAC). The anterior commissure is a tract connecting the two hemispheres (halves) of the brain. It’s crucial for interhemispheric communication, particularly in relation to smell, some aspects of memory, instinct, and emotion.
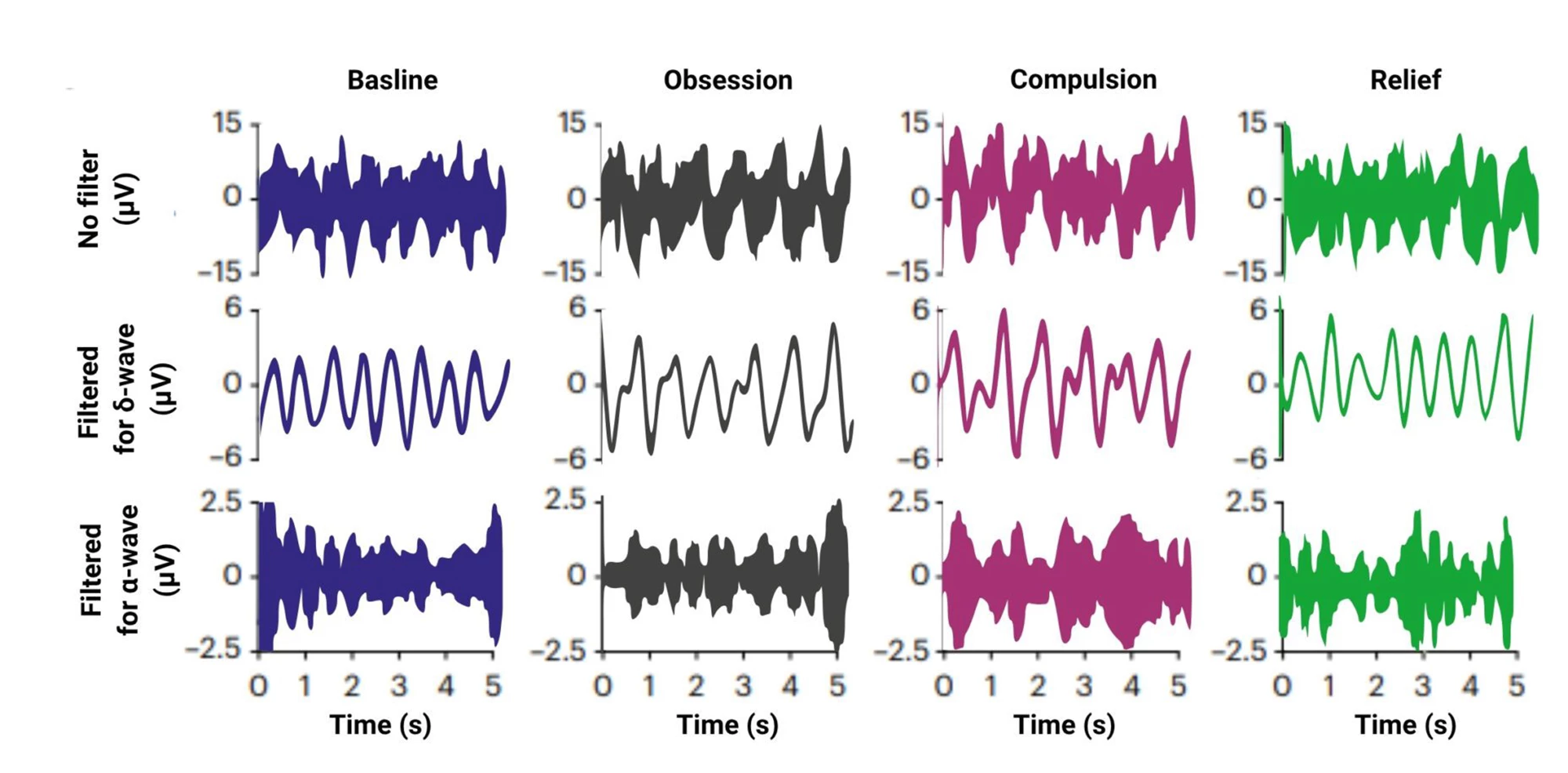
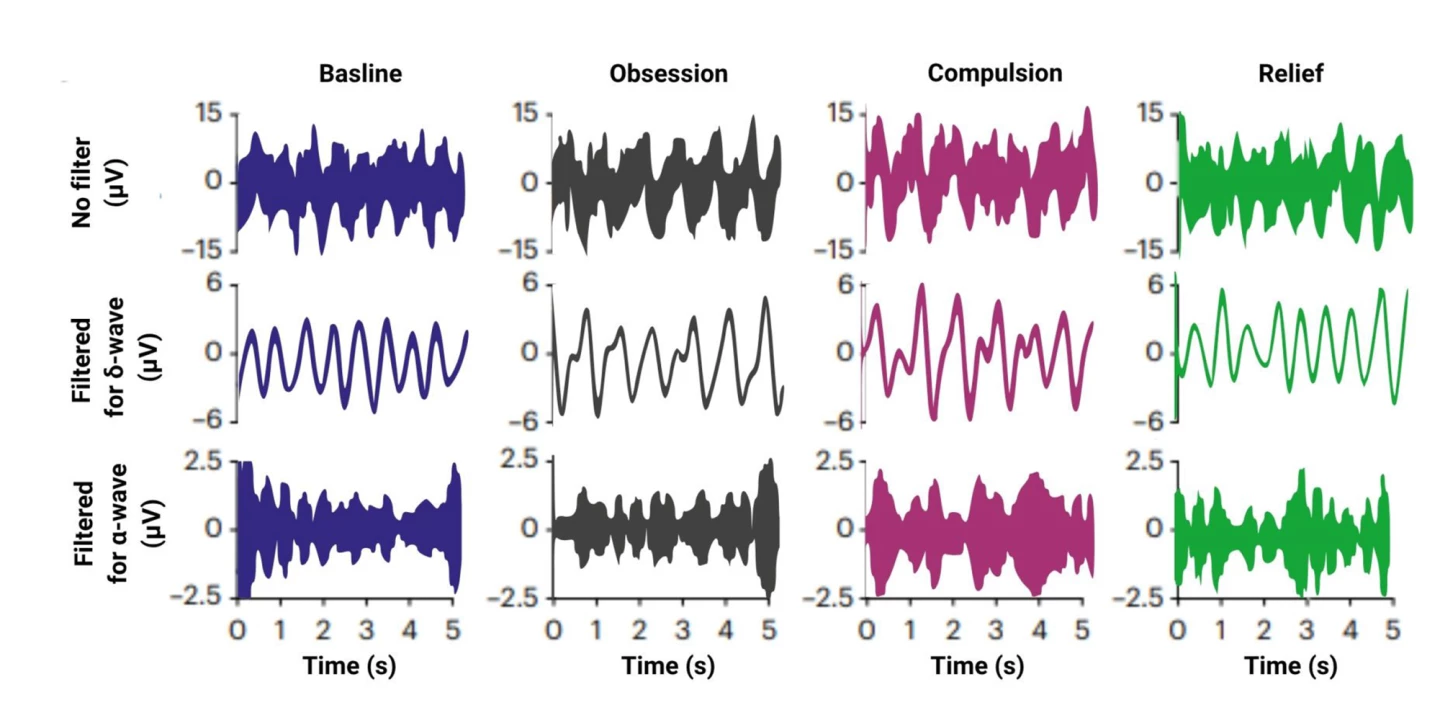
Our brains communicate using rhythmic electrical signals called brainwaves, which range from slow waves like delta (1–3 Hz, linked to deep focus or urgency) to fast waves like gamma (30–80 Hz, often tied to perception and cognition). Changes in these frequencies can reflect how the brain processes emotion, thought, and actions.
The researchers analyzed brain signals by region and frequency band (delta to gamma). OCD symptoms were self-reported using visual analog scales (VAS).
“What makes this study unique is that we were able to measure deep brain activity with very high spatial and temporal precision,” Arbab said. “That’s not possible with an fMRI [functional MRI] or EEG.”
The researchers found that across multiple brain areas, especially GPe and ALIC, delta and alpha (8–12 Hz, seen when a person is alert but relaxed) wave power increased significantly when patients performed compulsions. These increases were also seen in non-motor compulsions such as praying or thinking, suggesting the signals are related to the urge or compulsion itself, not just the physical act of performing it. In the anterior GPe, stronger delta waves during obsessions were positively correlated with how intense the patients rated their symptoms. During compulsions, anterior GPe delta power showed a non-significant trend toward decreasing as anxiety lessened.
The GPe and ALIC appeared to be more involved in the emotional and cognitive urge side of compulsions, while the NAc was more associated with motor actions. An abnormal interaction between theta (3.5–7.5 Hz, strong during internal focus, meditation and deep relaxation) and alpha waves was observed in ALIC only during compulsions. This interaction, known as phase-amplitude coupling, occurs when the timing (phase) of slower brainwaves influences the strength (amplitude) of faster ones. It’s thought to play a critical role in coordinating brain activity and enabling efficient information processing. In this case, the researchers suggest that the abnormal theta-alpha coupling may reflect a pathological neural signature of OCD.
“For the first time, we have found a clear biological marker for OCD in the brain, a marker that we may be able to use in future treatments for OCD,” Arbab said.
The study has some limitations. It was a small sample size of 11 patients; not enough to generalize across all types of OCD. Also, OCD is highly individualized, and while the study tailored obsessions/compulsions to each person, the diversity of symptom expression still limits conclusions. While the researchers compared motor and non-motor compulsions, non-OCD-related movement wasn’t controlled for, so some signals might still reflect motion. The study only examined subcortical brain areas; obsessions may be more strongly represented in cortical areas, which weren’t measured here. And subjective self-reporting via VAS may not fully capture the intensity or nature of symptoms like distress or disgust.
Regardless, the findings provide potential biomarkers that could be used to improve OCD treatment via DBS. It would provide a more personalized treatment that could improve efficacy and reduce side effects, compared to the current system of “always on” DBS.
“In the long term, we hope to switch to a system in which the electrodes only stimulate when they measure a signal that corresponds to compulsive behavior,” said Arbab. “That would make the treatment more targeted.”
The study was published in the journal Nature Mental Health.