Not only are surgical scars unsightly in many cases, but their limited elasticity can also reduce the patient's range of motion. There may be new hope, though, as a recent study has shed light on how a therapeutic peptide could drastically reduce such scarring.
Called alphaCT1 (short for "alpha Connexin Carboxy-Terminus 1"), the peptide was first created approximately 10 years ago by a team at Virginia Tech. Although its ability to reduce scarring was noted at the time, the means by which it's able to do so hadn't been fully explored until now.
In a recent double-blind study, a Virginia Tech team led by Prof. Rob Gourdie started by excising 5-mm punches of skin from the inner biceps of 49 healthy test subjects. Each person had one punch taken from each arm. The resulting wounds were then treated with topically applied gels – one wound on each person received a gel containing alphaCT1, while the other received a non-medicated gel as a control.
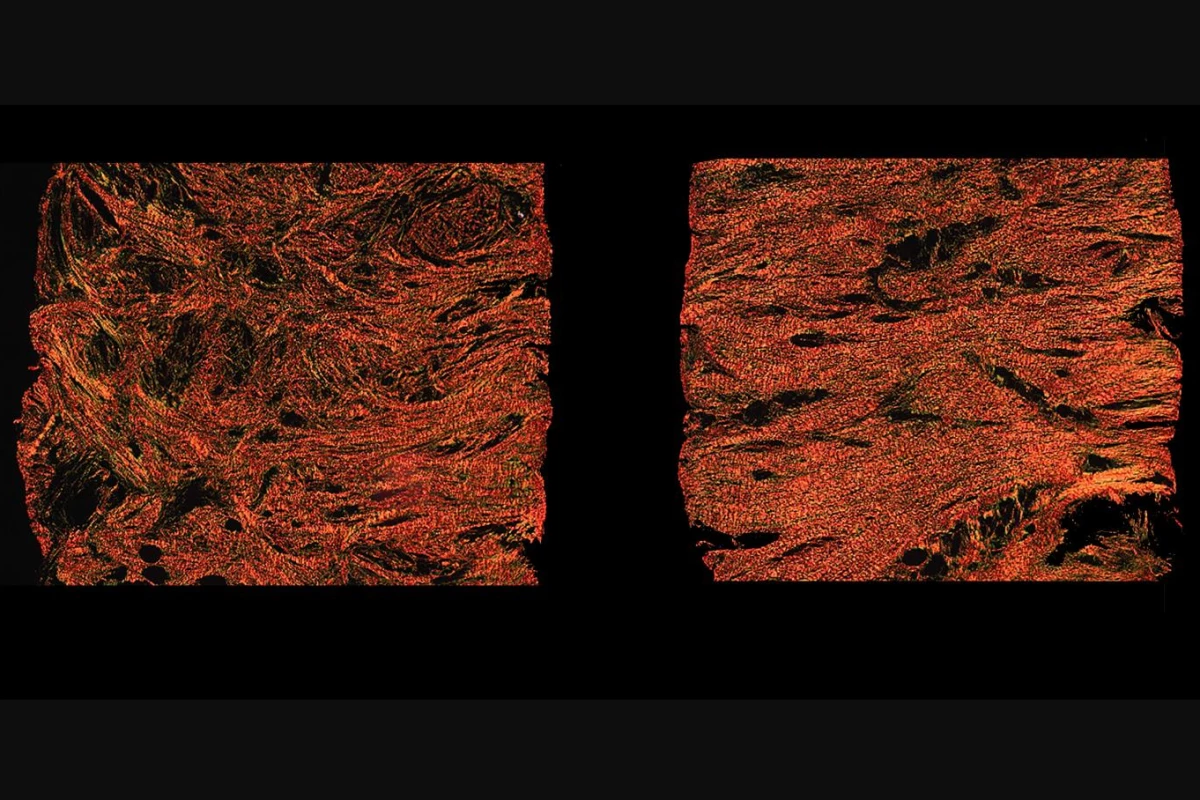
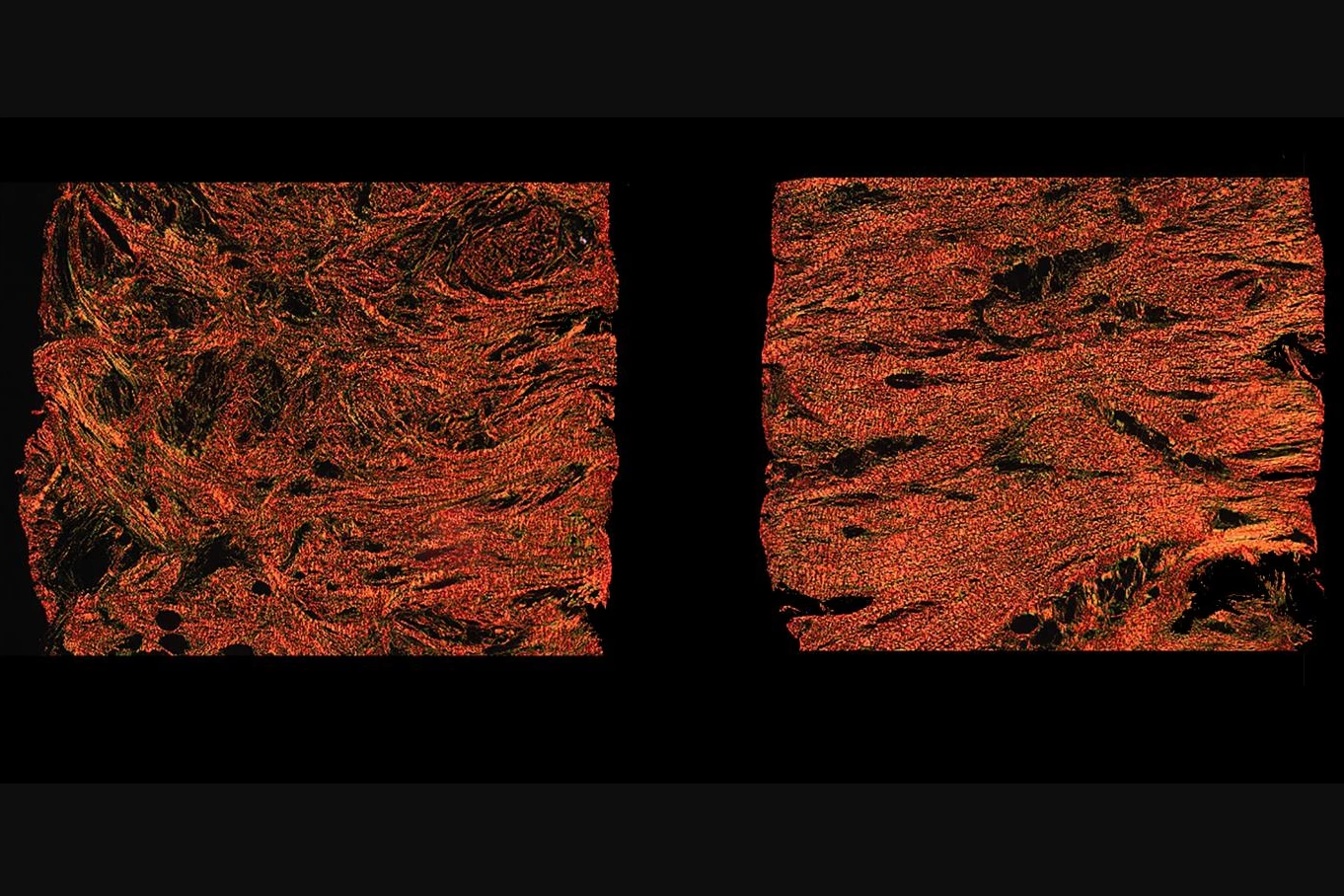
After a healing period of 29 days, the scars that formed on both wounds were photographed and biopsied for analysis. It was found that on the wounds treated with alphaCT1, the collagen that made up the scar took the form of enmeshed strips – this allowed the tissue to stretch in all directions, looking and behaving like unwounded skin.
By contrast, the wounds that were treated with the control gel produced much less pliable scars, in which the collagen strips were situated parallel to one another. Tests conducted on rats and guinea pigs produced similar results.
When human skin cell cultures were observed via a microscope, it was found that alphaCT1 caused collagen-producing cells known as fibroblasts to first stretch out like a rubber band, then snap back into their original shape and change direction. It is believed that this action, dubbed "the fibroblast dance," is what causes the collagen strips to become enmeshed.
AlphaCT1 is currently the subject of a phase 3 clinical trial, and is being commercialized by spinoff company FirstString Research.
A paper on the study was recently published in the Federation of American Societies for Experimental Biology (FASEB) Journal.
Source: Virginia Tech