An experimental drug under investigation as a potential cancer treatment has shown exciting potential in an entirely unrelated field of medicine, with scientists finding it confers benefits for weight loss and metabolic health in mice. These benefits were profound enough to surprise the authors of the study, who hope they could translate to a fast-acting but short-term treatments for obesity.
The drug in question is called ADI-PEG 20 and is currently being studied as a potential treatment for a range of cancers, such as sarcoma, breast and pancreatic cancers. It works by breaking down an amino acid in the blood called arginine, which robs cancer cells of an important fuel source. Studies have also shown that the gene activity behind the breaking down of arginine is greatly elevated when the body enters a fasting state.
The scientists at the Washington University School of Medicine in St. Louis therefore wondered if the drug could be used to mimic the effects of fasting, and conducted experiments in mice to explore the possibility. These revealed that the drug causes the cells to engage in a self-eating process called autophagy, in which they burn their own waste products for fuel. This is an effect observed during fasting when no new fuel is introduced into the body.
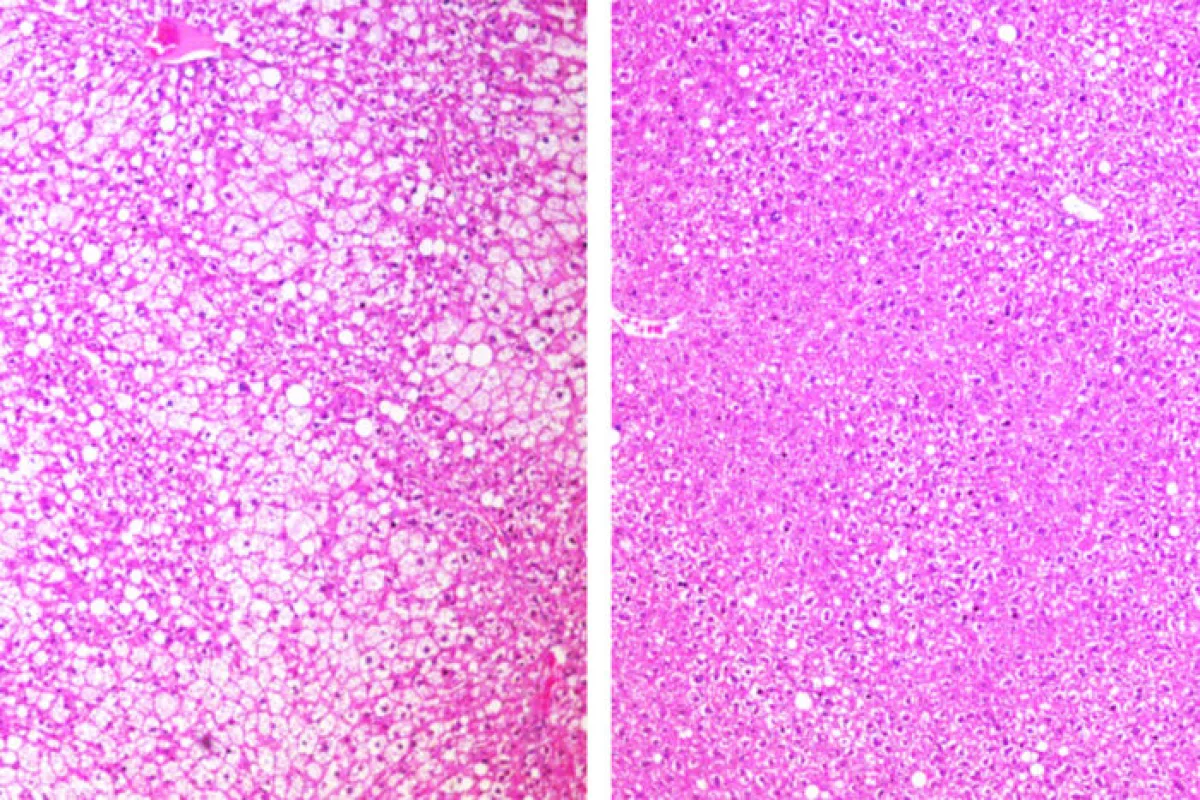
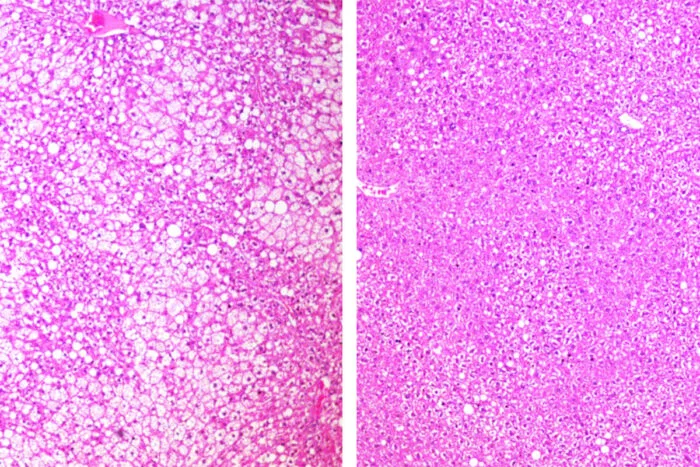
In mice genetically engineered to be susceptible to obesity, ADI-PEG 20 was found to protect them from typical weight gain, while it also caused weight loss in obese mice on high-fat, high-sugar diets. Additionally, it improved the rodents' cholesterol and insulin sensitivity, lowered inflammation and reduced fat buildup in the liver.
“Giving this drug seems to mimic some of the metabolic and therapeutic effects of fasting,” said senior author Brian DeBosch. “I was surprised by how large the effect was. In the mice prone to weight gain, the group that received the drug ended up weighing about 25 percent less than the mice that didn’t get the drug. And in the mice on the high-fat, high-sugar diet, we saw similar weight loss from the drug. Also, we don’t think that the preponderance of the drug’s metabolic benefits are from changes in body weight. In fact, for several outcome measures, the metabolic changes preceded significant changes in weight.”
Boding well for the drug's potential is that metabolic therapies tend to have fewer side effects than chemotherapy and radiation therapy, though clinical trials are still underway investigating its safety. One issue is that it is not a small molecule that could be taken for decades, but is a protein that could pose some problems, including an immune response over the long term. For this reason, the scientists see its immediate potential in short-term treatments.
“Many patients with obesity who are considering bariatric surgery must first lose some weight to make the procedure safer,” DeBosch said. “It can be difficult for such patients to lose up to 10 percent of their body weight before the surgery. This type of therapy could potentially serve as a bridge to help patients lose weight before bariatric surgery, to reduce the risk of complications during and after the procedure.”
The research was published in the journal Cell Reports Medicine.
Source: Washington University School of Medicine in St. Louis