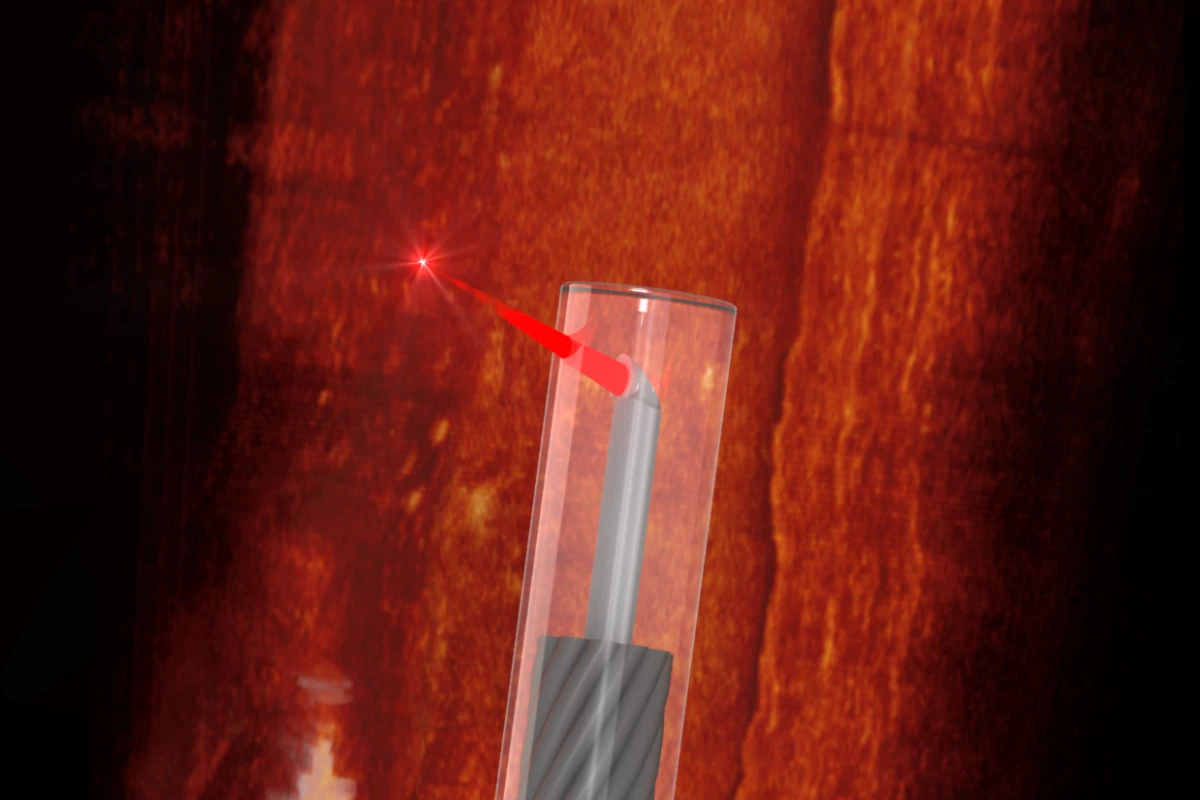
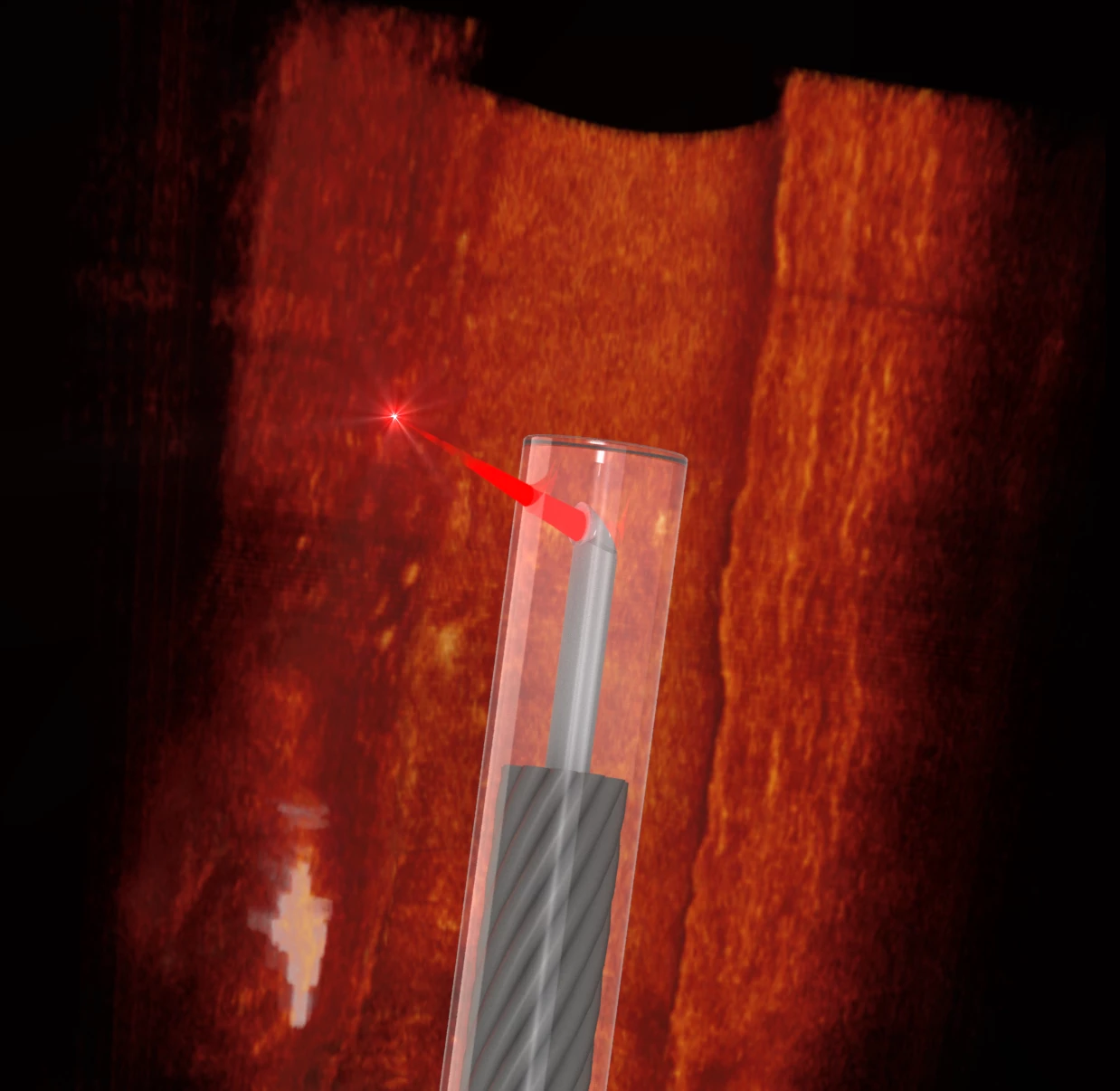
An Australian/German team has developed the world's smallest imaging device, at the thickness of a human hair. It's capable of traveling down the blood vessels of mice, offering unprecedented abilities to 3D-scan the body at microscopic resolutions.
To build this miniature endoscope, the team took a fine optical fiber with a diameter of less than half a millimeter (0.02 in), including its protective sheath. The researchers then used a 3D micro-printing technique to print a minuscule side-facing lens into it with a diameter less than 0.13 mm (0.005 in) – too small to be seen with the naked eye.
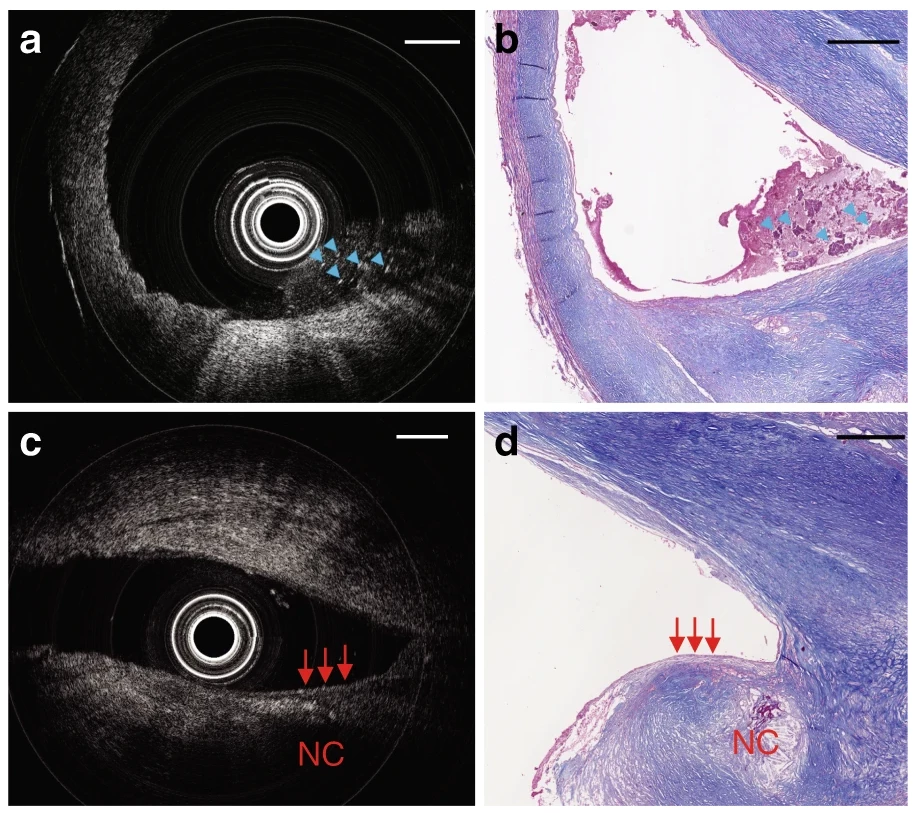
This optical fiber was then connected to an optical coherence tomography (OCT) scanner as a flexible probe. OCT is a 3D depth-sensitive scanning technology, commonly used to map the retina in optometry and ophthalmology. It uses near-infrared light to penetrate into tissue, measuring the wave interference between a reference beam and a probe beam to build up live 3D images that can look through surfaces within the body into the structures beneath at microscopic resolutions.
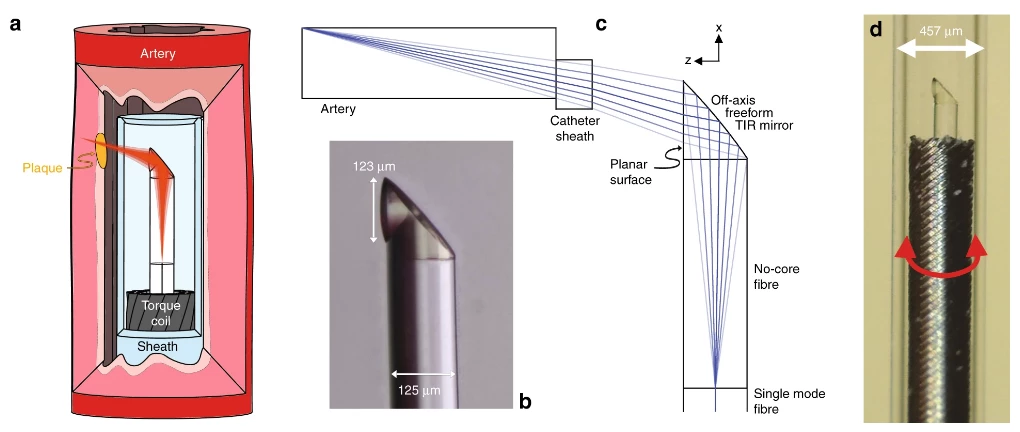
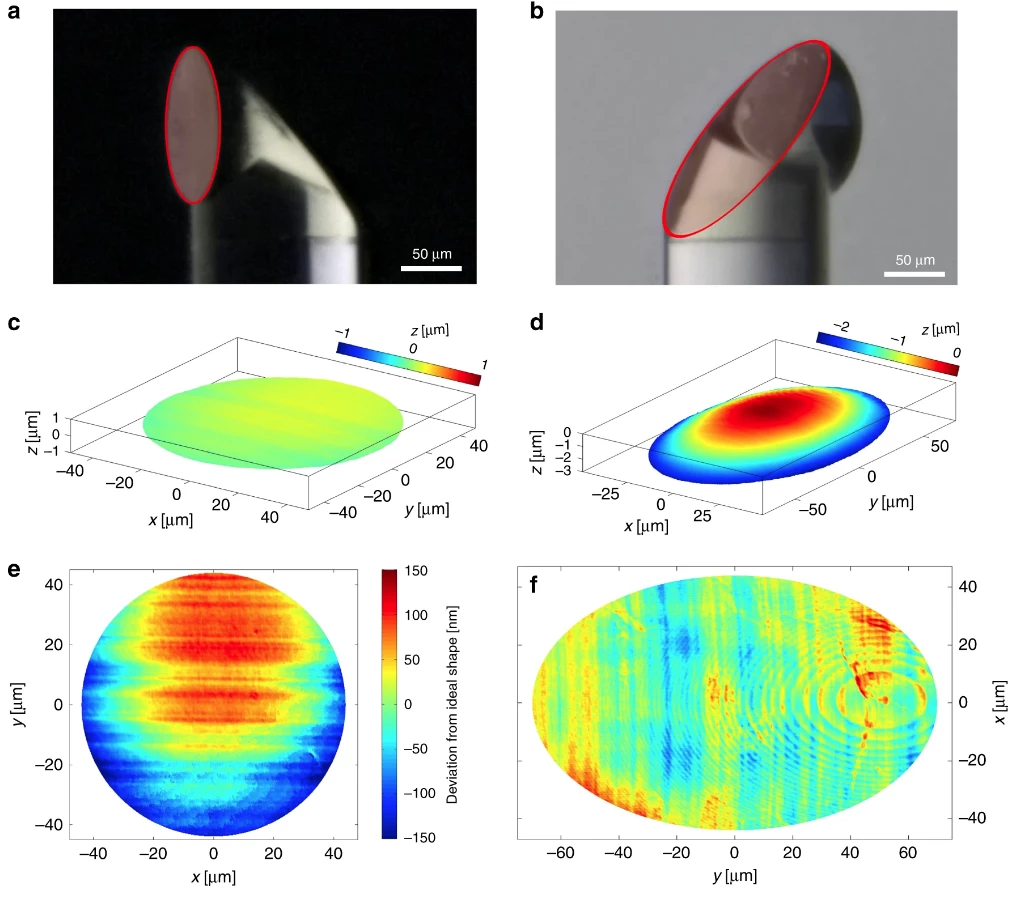
b.) Microscope image of the 3D-printed off-axis freeform total internal reflection (TIR) mirror on the tip of the no-core fiber that is fusion spliced onto the light-guiding single-mode fiber.
c.) Optical design of the system with light exiting the single-mode fiber, expanding in the no-core fiber, being reflected and phase-shaped at the freeform mirror, passing the catheter sheath and focusing into the artery tissue.
d.) Photo of the 3D-printed OCT endoscope, which rotates and is pulled back to accomplish full 3D OCT scanning
With this breakthrough, the team has built an OCT scanning device small enough to be pushed through blood vessels in the body. This ultra-thin probe can be rotated and slowly pulled backwards to build up a 3D map of its surroundings to a depth around half a millimeter below the surface. It offers unprecedented abilities to scan the vascular system of the body for the plaques, made up of fats, cholesterol and other substances, that tend to build up in blood vessel walls and lead to heart disease.
The team performed successful tests of the device in both human and mouse blood vessels, demonstrating its ability to deliver quality OCT images and the flexibility to get where it needs to go in the body. Its precisely printed lens allows the scanner to image depths five times deeper than previous attempts, and the researchers believe this tiny probe could open up new scanning options in hard-to-reach places like the cochlea of the ear and potentially even parts of the nervous system.
The team comprised medical clinicians and engineers from the University of Adelaide and the University of Stuttgart.
The study is available in the journal Light Science & Applications.
Source: University of Adelaide