Fascinating new research from scientists at Johns Hopkins University is shedding light on the mystery of how deep brain stimulation improves physical symptoms in Parkinson’s disease patients. The study reveals evidence for the first time suggesting the electrical stimulation technique directly increases dopamine release in the brain.
"While deep brain stimulation has been used for treating Parkinson's disease for more than three decades, the mechanism of action is not fully understood," explains Gwenn Smith, from the psychiatry and behavioral sciences department at Johns Hopkins University School of Medicine.
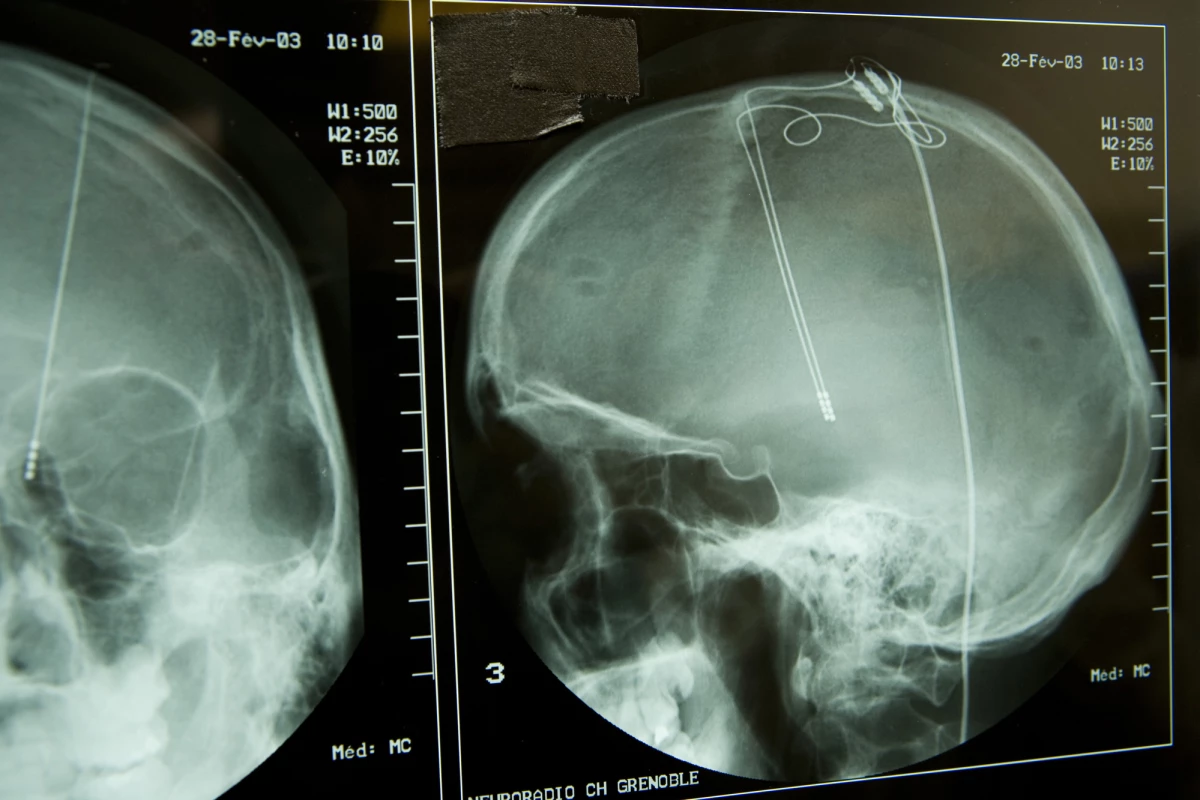
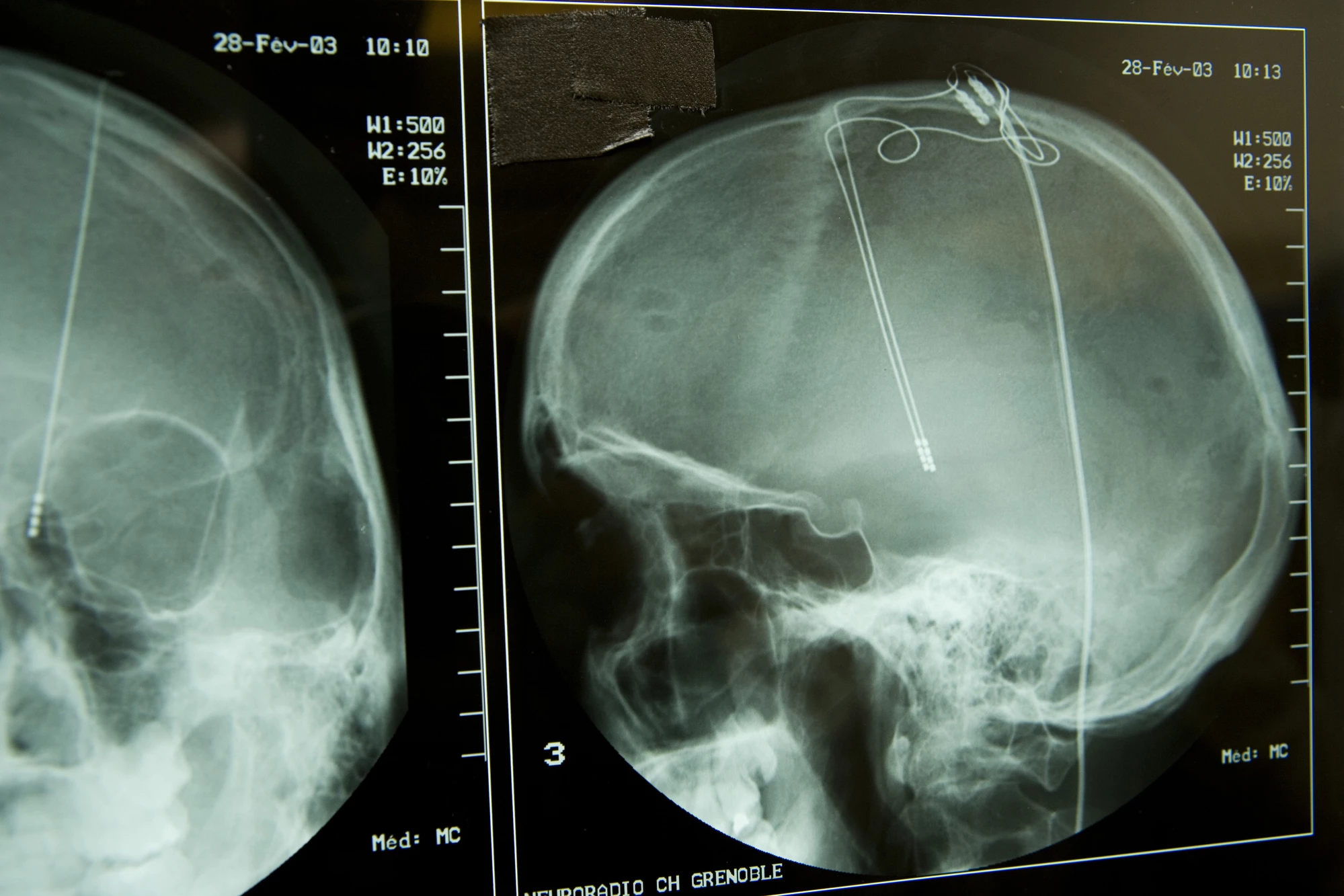
Deep brain stimulation (DBS) has been used to treat symptoms in Parkinson’s disease sufferers for several decades. The treatment involves several tiny wires being implanted into a patient’s brain, primarily targeting areas connecting to the ventral thalamus. Applying sporadic electrical currents directly to certain parts of the brain has been found to consistently reduce symptoms including tremors, muscle stiffness and slowed movement.
The main drug currently used to treat Parkinson’s disease is called levodopa. It works by helping cells in the brain produce more dopamine. So while it wouldn’t be unreasonable to assume DBS also works by increasing levels of dopamine in the brain, scientists have never been able to effectively prove this. This has led other researchers to hypothesize DBS’s mechanism of action to possibly work by inhibiting neuronal activity in certain areas of the brain. However, the Johns Hopkins team still hypothesized dopamine release as being a major part of DBS's mechanism of action.
"We knew that dopamine-producing cells get connections from many parts of the brain," says Kelly Mills, another researcher working on the project. "So, even if dopamine-producing cells are not activated directly, electrically stimulating other parts of the brain—particularly those that receive information from dopamine-producing cells—can indirectly increase dopamine production. But supporting evidence in patients was generally lacking."
Instead of focusing directly on dopamine levels, the researchers looked at another molecule that interacts with dopamine, called vesicular monoamine transporter (VMAT2). This molecule plays a key role in dopamine transport around the brain, and prior research has indicated a clear inverse relationship between dopamine and VMAT2. So basically, when dopamine levels in a brain rise, VMAT2 levels drop.
Seven Parkinson’s patients, with implanted DBS electrodes, were administered PET scans before and after electrical stimulation was applied. Symptoms were evaluated following the application of DBS to verify the process had worked, and analyzing the PET scans did indeed reveal VMAT2 levels dropped following the electrical stimulation.
The correlation between VMAT2 levels dropping and symptomatic improvements following the electrical stimulation suggest an increase in dopamine levels may be a key mechanism in explaining how DBS works in Parkinson’s patients.
"We were able to see an increase in dopamine levels because we changed the way we looked at the problem," says Mills. "Rather than looking at the amount of dopamine bound on receptors of dopamine-receiving cells, we looked at VMAT2 concentrations within dopamine-producing cells, which may be more sensitive to detecting changes in dopamine with deep brain stimulation in Parkinson's disease patients."
This research is the first time dopamine release has been empirically implicated in the efficacy of DBS in Parkinson’s disease patients. Although currently this form of targeted electrical brain stimulation is only truly effective by surgically implanting electrodes into a brain, researchers are working on various new methods to achieve similar results with non-invasive techniques.
"In the long term we want to have a broader idea of the effects of electric stimulation on brain function and chemistry so that we can better treat Parkinson's disease and other neurological and psychiatric conditions, like Tourette's syndrome and depression, which are also affected by the dopamine system," says Smith.
The new study was published in the journal Parkinsonism & Related Disorders.
Source: Johns Hopkins University