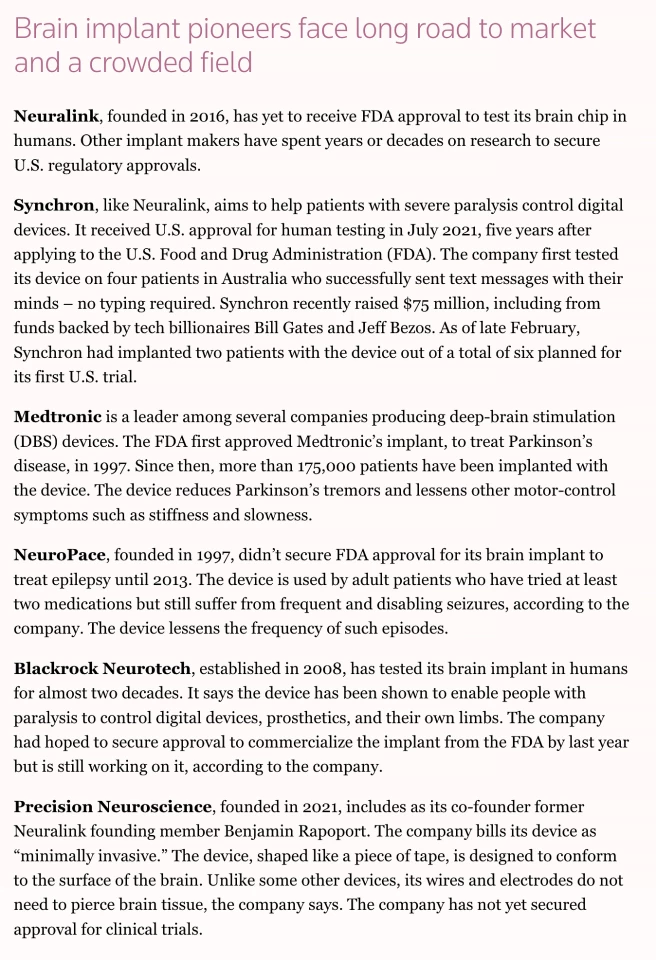
Huge advances in medical technology have led to increasingly advanced implanted neurological devices, such as deep brain, vagal nerve, and spinal cord stimulators. Elon Musk’s Neuralink, a wireless brain-computer interface (BCI), is one of the more well-known devices. China recently unveiled its own BCI implant, indicating that it’s quickly catching the US in the neurotechnological space.
Implanted neurotech devices have improved the quality of life of people living with neurological conditions. But, given the speed of advancement we’re currently seeing, what happens when the implanted neurotech quickly becomes obsolete? Or no longer receives maintenance support from its manufacturer (think of Windows withdrawing support for outdated versions of its operating system)? Can it be removed, and if so, who pays for that?
It boils down to this: Should protections be in place to cover these situations? Some argue that, yes, they should be. In a recently published paper, a study led by researchers at the Norman Fixel Institute for Neurological Diseases in Florida, US, proposed a formal definition of ‘implanted neurological device abandonment’ that, they say, is important for developing guidelines, policies and laws relating to implantable neurotechnological devices.
Neurotech implanted as part of a clinical trial
In 2020, Nature Medicine reported the story of Australian woman Rita Leggett, who’d received an experimental brain implant to treat her epilepsy. Implanted as part of a clinical trial, the device worked for Leggett: she stopped having seizures. However, mid-way through the trial, NeuroVista, the company that made the device, folded after investors became nervous about providing financial backing to such invasive technology.
Because the company was no longer operating, there was no means of monitoring the device. It was, quite literally, dead in Leggett’s head (well, not quite – the battery was meant to last three years). Her husband offered to buy the device from NeuroVista but was refused because of its proprietary components. Her only option was to have the device removed or ‘explanted’.
According to Frederic Gilbert, an associate professor at The University of Tasmania who specializes in the ethics of neurotechnology and was interviewed for the Nature Medicine article, removing a device can be tantamount to withdrawing treatment. Gilbert said that’s because these devices can profoundly affect a patient’s identity. The distress caused by the device’s removal may be directly proportional to the tech's effectiveness.
The authors of the current study formed the view that, on its face, clinical trial failure wasn’t neurotechnological device abandonment chiefly because failure can result from safety concerns or a lack of therapeutic effect. However, they said it’s essential for those running a clinical trial to satisfy three criteria to stay on the ‘right’ side of abandonment. First, study participants should be informed about the potential for discontinuance of the trial and that they’ll be assigned to treatment or control arms of the investigation. Second, participants should be notified if and when a trial will be discontinued. Finally, participants should be provided with resources for other therapeutics that meet accepted standards of care.
Of course, in addition to the issue of trials being terminated prematurely, there’s the issue of what happens to a neurotech implant when a trial reaches its natural conclusion. In that situation, device removal is usually offered to participants. However, it’s typically after researchers have contacted their public or private health insurance companies to see whether they’ll cover the cost. There are no clear, current guidelines regarding whether an implant stays in or is removed.
The collapse of neurotechnology companies
The worldwide market for neurotechnological products is expected to reach US$17.1 billion in 2026. However, that does not guarantee that companies making these products will stay afloat. NeuroVista isn’t the only neurotech company that has closed its doors to consumers.
In 2019, Autonomic Technologies (ATI) stopped operations following successful placebo-controlled trials of its stimulator, which treats cluster headaches. Granted, the company closed due to regulatory fraud, but the outcome for the more than 700 people who used the device was the same: they couldn’t access the proprietary software needed to recalibrate it and maintain its effectiveness. Luckily, Unity HA acquired ATI’s intellectual property and, in 2022, was granted Breakthrough Device designation by the FDA.
Nuvectra, a manufacturer of a spinal cord stimulator for chronic pain, filed for bankruptcy in 2019. The same year, artificial-vision company Second Sight started hemorrhaging money and advised implantees that they were stopping production of their retinal implants to focus on brain implants to restore vision. In early 2020, the CEO and director of research and development exited suddenly, most employees were laid off, and the company started auctioning its physical assets, leaving 350 or so people fitted with a Second Sight implant to wonder what was happening. The company merged with Nano Precision Medicine (NPM) shortly after. In mid-2020, another manufacturer of spinal cord stimulators, Stimware, recalled all its devices and, in 2022, filed for bankruptcy. There’s bound to be more.
When companies like these go under, the implants they created are typically left in place. In most cases, explantation is deemed too expensive, too risky, or simply unnecessary. So, for people with neurological conditions, it’s back to the drawing board – albeit carrying an additional piece of (useless) hardware.
If they’re lucky, they can find a replacement device. According to an article published in Nature in 2022, replacing obsolete implants like Nuvectra’s spinal cord stimulator requires surgery that takes weeks to recover from. Plus, it’s expensive. The surgery and replacement device will set you back around US$40,000. And that’s assuming there is a replacement device available.
Device longevity: to remove or not to remove
As has already been mentioned, a neurotech device considered cutting-edge today may not be cutting-edge tomorrow. These devices have an in-built expiration date, at which point they stop being functional and effective without ongoing maintenance and support.
In the summer of 2020, Elon Musk shared a progress update about the Neuralink implant. Describing the device as a “Fitbit in your skull,” Musk was characteristically blasé when describing the insertion process he envisioned eventually using on humans.
“Essentially, you open a piece of skull,” he said. “You remove about a coin-sized piece of skull, and then the robot inserts the electrodes … Then the device replaces the portion of skull that was removed. And we basically close that up with, actually, super glue, which is how a lot of wounds are closed. And then you can just walk around right afterwards. It’s pretty cool.”
Yeah, cool. But what was more interesting was the section of the presentation that concerned Dorothy the pig, who used to have a Neuralink. Musk said that removing Dorothy’s implant demonstrated the device’s “reversibility.”
“What Dorothy illustrates is that you can put in the Neuralink, remove it, and be happy, healthy, and indistinguishable from a normal pig,” said Musk.
That's all Musk offered on the device's removal. Nothing about its risks. The full 2020 Neuralink progress update is available below.
Musk’s brain implant company has since moved on from pigs and begun recruiting for its first human trial. But it first had to fight the FDA for approval. Reuters reported in 2023 that the agency rejected an application for trial approval on the grounds of patient safety, citing major concerns about, among other things, how the device could be removed without damaging brain tissue. Musk has his approval now, so the FDA appears to be satisfied.
It's difficult to find expert commentary on whether removing Neuralink – or another brain implant – will or will not damage the brain. To be fair to Musk, without human subjects, it may be unfair to speculate at this stage. But, if implanting a device like Neuralink carries a risk of causing damage to brain tissue, it would be reasonable to assume that removing it does, too.
A definition of ‘implanted neurological device abandonment’
To inform their study, the researchers reviewed articles on neurological device abandonment before reaching a consensus on an appropriate definition. They propose the adoption of a standard definition, which comprises one of the following:
- Failure to provide information relevant to (the existence or absence of) plans for medical, technical, and/or financial responsibility as fundamental aspects of patient consent during and after a clinical trial.
- Failure to fulfill reasonable responsibility for medical, technical, and/or financial support prior to the end of an implantable device’s labeled lifetime.
- Failure to address any immediate needs (e.g., infection or device reprogramming) of the individual using the implanted device, which may result in safety concerns and/or the deterioration of device effectiveness.
- Failure of a clinical research trial if or when (1) informed consent has failed to address ongoing access to and management of the implanted device (per 1, above) and/or such other devices that may be demonstrated as having equal or greater therapeutic value in the future and (2) individuals responsible for the trial have not made a reasonable effort to facilitate continued access to device and support for patients who benefit from the device.
The issues raised in this article make it clear that greater, more consistent guidance is needed in this rapidly evolving field to protect patients and their medical practitioners.
“We opine that these tenets previously listed may afford a working basis for further consideration, discourse, and dialogue toward establishing a formal definition of abandonment of active implantable neurotechnological devices and guidelines, policies, and laws to prevent its occurrence,” said the researchers.
The study was published in the journal JAMA Network Open.








