Researchers have found a genetic link between the nighttime production of the sleep hormone melatonin and ADHD symptom severity in children. The study enhances our understanding of the complexities associated with this prevalent neurodevelopmental condition.
Sleep disturbances, including insomnia, restless sleep, and daytime drowsiness, are common in people with attention-deficit hyperactivity disorder, or ADHD. It’s been hypothesized that people with the condition have a disrupted circadian rhythm. However, the exact mechanism connecting sleep problems and ADHD has remained elusive.
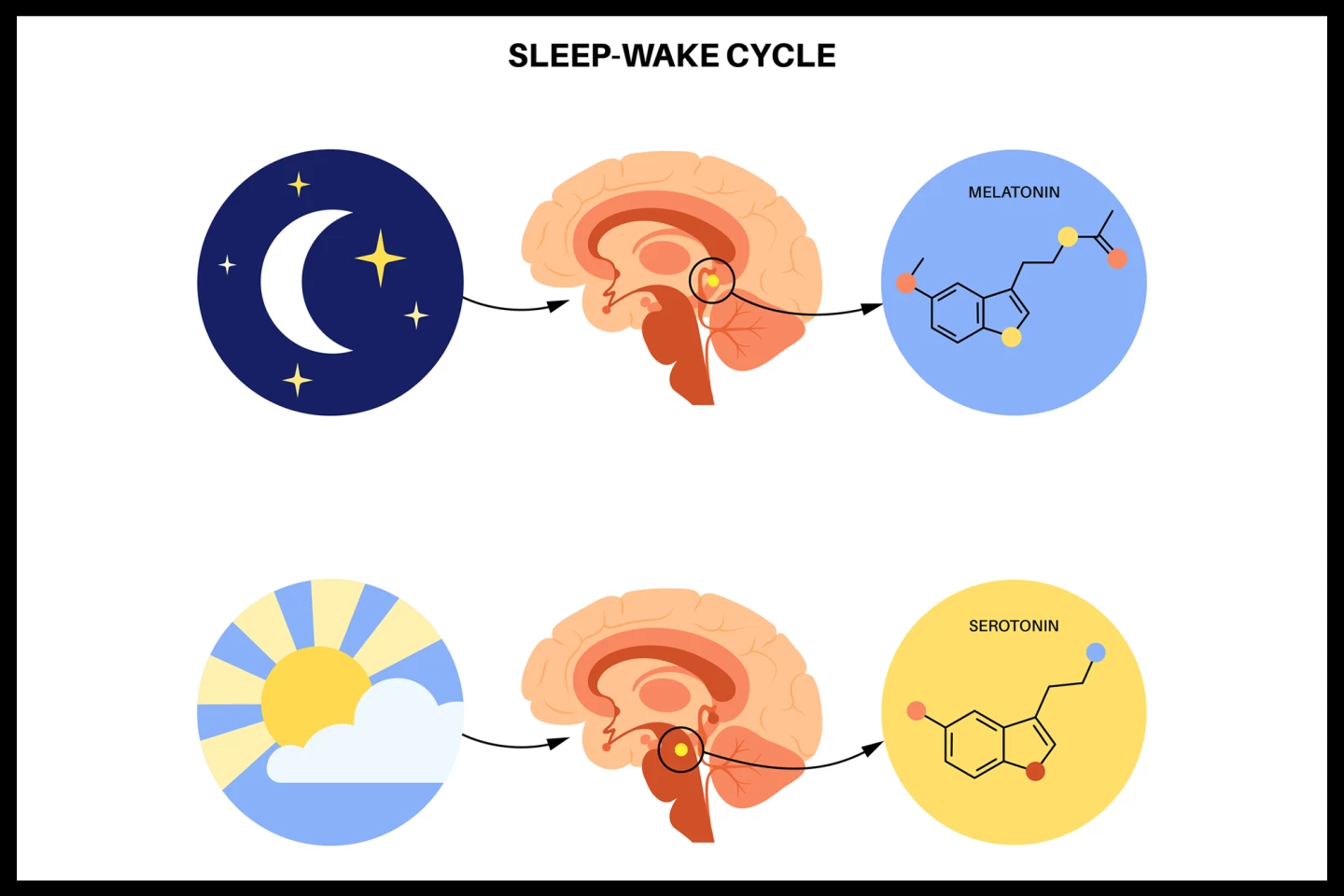
A new study led by the Nagoya University Graduate School of Medicine in Japan may have provided the answer. The researchers found an association between the production of melatonin at night, a naturally produced hormone that regulates the body’s sleep-wake cycles, and the severity of ADHD symptoms in children.
“Our findings indicate that disruptions in melatonin secretion may contribute to the difficulties children with ADHD face in maintaining regular sleep patterns,” said lead and corresponding author Associate Professor Nagahide Takahashi, MD, PhD, from the Department of Child and Adolescent Psychiatry at Nagoya University Graduate School of Medicine.
The researchers obtained data from three different study cohorts. One was the Danish iPSYCH study, which included data from 14,584 participants diagnosed with ADHD and 22,492 participants without ADHD. Second, data on 2,373 adults obtained from the Taiwan Biobank, which was used to analyze genetic markers related to melatonin secretion through a measure called UMCR (urinary 6-hydroxymelatonin sulfate-to-creatinine ratio). And, finally, the Japanese Hamamatsu Birth Cohort (HBC) study, which included 729 children aged eight to nine years with both genetic data and ADHD symptom scores.
The researchers used UMCR as a proxy for nighttime melatonin secretion. They also measured ADHD symptoms, children’s sleep behaviors, and polygenic risk scores (PRS), which are a way of estimating an individual’s predisposition to a particular disease or trait, based on the combined effect of many small genetic variations. After analyzing these measures, they found a statistically significant genetic correlation between lower melatonin secretion and higher ADHD risk. In the HBC cohort, kids with a higher genetic risk for reduced melatonin had more ADHD symptoms, especially inattention. While the kids with higher melatonin-related genetic risk had more delayed sleep onset (the time it takes to fall asleep), the analysis showed that this didn’t explain the link between genetics and ADHD symptoms. This suggests that the genetic effect is direct, rather than being solely due to poor sleep habits.
The researchers then sought to gain a deeper understanding of the biology underlying the connection between melatonin secretion and ADHD symptoms by examining levels of the inflammatory messenger interleukin-6 (IL-6) in the children’s blood. Previous studies have found that children with ADHD have significantly elevated IL-6 levels, suggesting it might contribute to the development of the condition. IL-6 and melatonin have a complex relationship, with melatonin potentially regulating IL-6 levels and influencing its anti-inflammatory effects. In the current study, several immune-related pathways, particularly those involving IL-6, were found to be associated with both melatonin secretion and ADHD.
Taken altogether, the study’s findings suggest that melatonin secretion and ADHD are genetically linked, and this relationship appears to go beyond bad sleeping habits. The immune system, particularly IL-6 signaling, might play a role in this connection.
There are limitations to the study. The researchers didn’t measure actual melatonin or UMCR levels in the Japanese cohort, only the genetic risk. They also didn’t have a second cohort to confirm the PRS results, so these findings need to be replicated in another study. In short, more research is needed to solidify the mechanisms indicated by the current study.
Regardless of these limitations, the study’s findings have improved our understanding of the complex interplay between sleep and neurodevelopmental disorders like ADHD. Further, they’re important from a practical perspective.
“These findings suggest that children with ADHD diagnosis/symptoms may struggle to maintain their circadian rhythm due to a disrupted melatonin secretion system,” the researchers said. “This also highlights the important of practicing good daily sleep habits and sleep hygiene to increase and regulate melatonin levels at night during early childhood to minimize ADHD symptoms”.
The study was published in the journal Psychiatry Research Communications.
Source: University of Osaka







