By obtaining high-resolution images of Alzheimer’s disease-affected brain cells as the condition progresses, researchers have identified the specific neurons that are damaged. The information the ‘cell atlas’ provides highlights potential new treatment targets.
After identifying that accumulation of toxic tau and amyloid proteins in the brain are a feature of Alzheimer’s disease, researchers have, understandably, been working on treatments that reduce or eliminate them. Less research has focused on the specific cells affected by the condition.
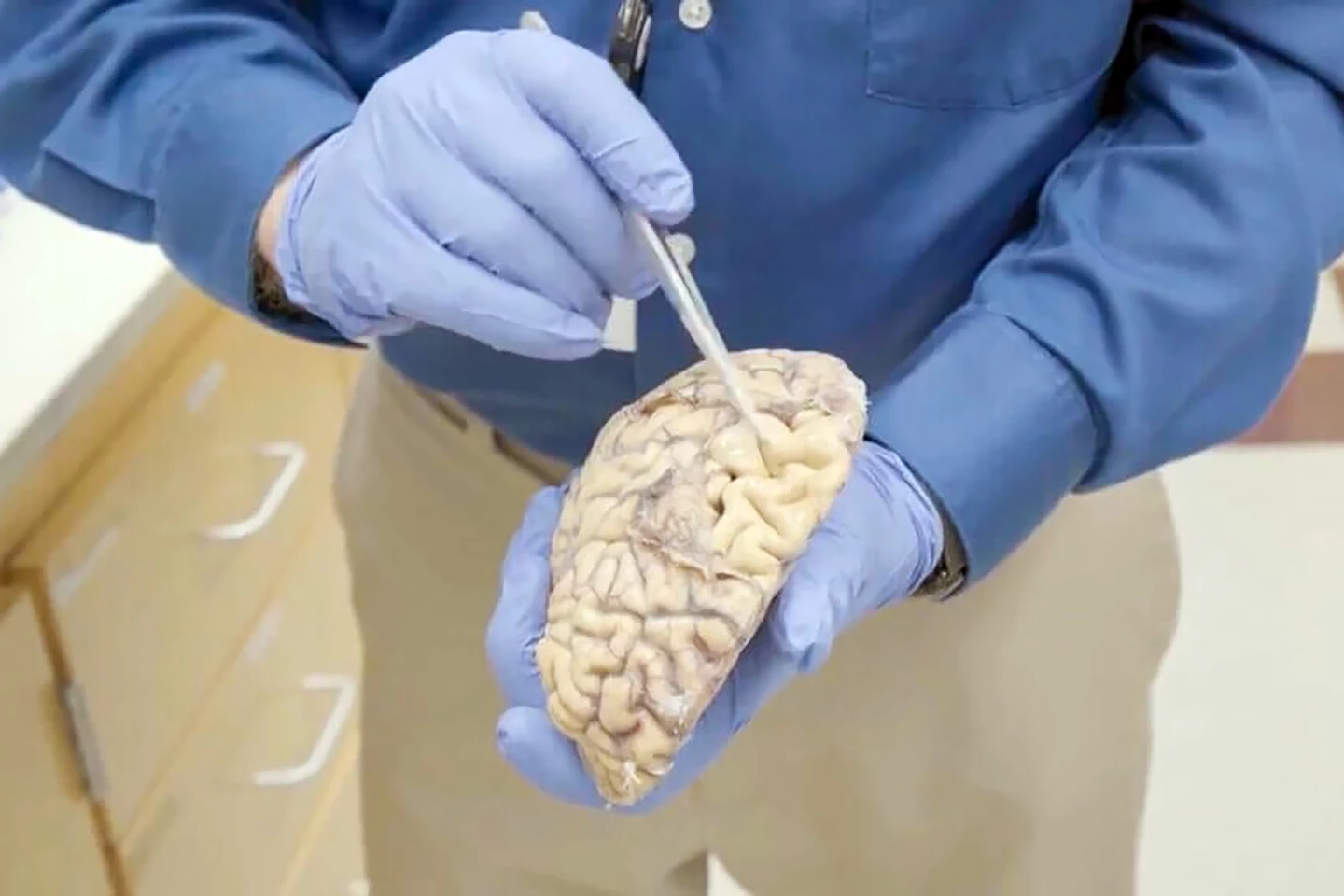
Now, researchers from the Allen Institute for Brain Science, the University of Washington (UW) Medicine, and the Kaiser Permanente Washington Health Research Institute have created a high-resolution timeline of images that show how Alzheimer’s disease progresses at the cellular level.
“The takeaway is that this atlas describes AD [Alzheimer’s disease] progression at unprecedented cellular resolution, and identifies many new cellular and molecular targets for the field to explore,” said Kyle Travaglini, PhD, a scientist at the Allen Institute and the study’s co-lead author.
The researchers zeroed in on cells from a particular region of the brain’s outer layer, or cortex, called the middle temporal gyrus (MTG), which is involved in language, memory processing, and visual perception. The MTG is also a critical ‘transition zone,’ where preclinical Alzheimer’s pathology, such as the buildup of toxic proteins, transitions to more advanced dementia-related neurodegeneration.
Over 3.4 million cells from 84 research participant donors at different stages of Alzheimer’s progression were examined using single-cell and spatial genomics technologies to map the active genes, DNA structure and precise location of individual cells in the MTG of donors. These data were compared to a massive brain reference map that’d already been generated by the Allen Institute team and collaborators at the National Institutes of Health’s (NIH) Brain Research through Advancing Innovative Neurotechnologies (BRAIN) Initiative – Cell Census Network or BICCN.
“By studying research subjects across the spectrum of AD, including those in the earliest stages of disease, we hope to identify vulnerable cells early in the disease process, long before a person develops symptoms,” said C. Dirk Keene, professor and chair in neuropathology at UW Medicine and a co-corresponding author on the study.
Machine learning was used to align the two datasets and construct a high-resolution view of how Alzheimer’s disease affects different cell populations over time.
“You could say that we created a pathology clock that tells not only what changes are happening in this cortical region, but when,” said Mariano Gabitto, PhD, the other lead author and an assistant investigator at the Allen Institute. “We now have a framework to arrange the sequence of events as Alzheimer’s pathology increases over time.”
The researchers observed two distinct phases of Alzheimer’s disease: the slow, early buildup of abnormal cellular changes that occur before the onset of memory issues or cognitive impairment, followed by a later, rapid increase that coincides with cognitive decline.
The early phase was marked by inflammatory changes in the brain’s immune cells (microglia) and support cells (astrocytes). This wasn’t surprising given that previous studies had implicated these non-neuronal cells. What was surprising was that a specific type of neuron in the MTG, somatostatin-expressing inhibitory or SST neurons, were some of the earliest casualties of the disease.
To date, most research has focused on microglia and the loss of excitatory neurons. By way of explanation, neurons communicate through electrical currents called action potentials, which can be excitatory or inhibitory. Excitatory currents prompt one neuron to pass information on to the next through an action potential; inhibitory currents reduce the likelihood that information will be passed on.
The early phase also saw a loss of oligodendrocytes, cells that insulate nerve fibers and help facilitate communication in the brain, in the cortex. That loss caused the activation of a repair pathway to restore the nerve insulation. The later phase involved much more extensive neuronal loss, including specific types of inhibitory and excitatory neurons. Interestingly, the cell loss was concentrated in the upper layers of the cortex.

From their findings, the researchers hypothesize that the loss of these cells may trigger a domino effect that upsets the delicate balance between inhibition and excitation, promoting widespread system failures that result in neuronal loss and cognitive decline. This view of Alzheimer’s disease as a 'circuit disorder' challenges the thinking that pathological proteins are solely responsible.
“The initial triggers of disease may involve pathological proteins or microglial activation, but it is loss of specific types of neurons and the connections they make that lead to cognitive decline,” said Ed Lein, PhD, senior investigator at the Allen Institute and the study’s co-corresponding author.
In addition to providing a high-res visual timeline of the disease’s progression, the study also identifies potential new treatment targets.
“Armed with this information, maybe we could target not only molecules like tau and amyloid, but also vulnerable cell types,” Lein said. “Perhaps we could protect them and prevent their degeneration – and the whole downstream cascade of events.”
The Allen Institute, UW Medicine, and Kaiser Permanente Institute together form the Seattle Alzheimer’s Disease Brain Cell Atlas (SEA-AD) consortium, a community resource that makes its open-source data available to students, researchers, and clinicians.
The study was published in the journal Nature Neuroscience.
Source: Allen Institute







