An unusual partnership between a vacuum maker, a race car legend, and the University of Edinburgh is leading to advances in understanding dementia. Their new study using living tissue has revealed the brain's sweet spot for tau proteins.
After his wife was diagnosed with dementia in 2014, legendary Formula One driver Sir Jackie Stewart founded an organization known as Race Against Dementia (RAD), which funds researchers who are just starting out in their search for a cure for cognition-impairing diseases like Alzheimer's and other forms of dementia.
More recently, the James Dyson Foundation linked up with RAD via a £1.5 million 5-year grant to fund the work of the RAD Dyson Fellow, Dr. Caire Durrant, from the University of Edinburgh. That partnership is already paying dividends, as evidenced by new research published by Durrant's team in the journal Nature Communications.

Using living human brain tissue, the researchers set out to study what happens when our brains encounter a toxic form of amyloid beta, a protein that's a building block of the amyloid plaques that build up in the brains of Alzheimer's patients. While it's no longer thought that these plaques cause Alzheimer's disease, they are certainly a key symptom, with their accumulation in the brain gunking up communications between neurons.
Durrant and her team found that when exposed to the toxic amyloid beta, the brain tissue simply didn't attempt to repair itself. They also discovered that even small changes to the normally occurring levels of amyloid beta in the brain – either higher or lower – was enough to disrupt the normal function of brain cells, leading them to conclude that there is a sweet spot where the protein can function correctly and not cause damage. The researchers say the finding should allow them to zero in on drugs that have the best chance of both maintaining these levels and reducing neuronal damage.
As part of the research, the team also found that slices of brain tissue taken from the temporal lobe released high levels of another Alzheimer's-implicated protein: tau. Tau also has the unfortunate ability to form clumps known as tangles in the brain, again interfering with normal cellular communication. Finding it in this brain region, which is associated with the formation of auditory and visual memories, could explain why the temporal lobe is particularly affected early in the disease's progression.
It's alive!
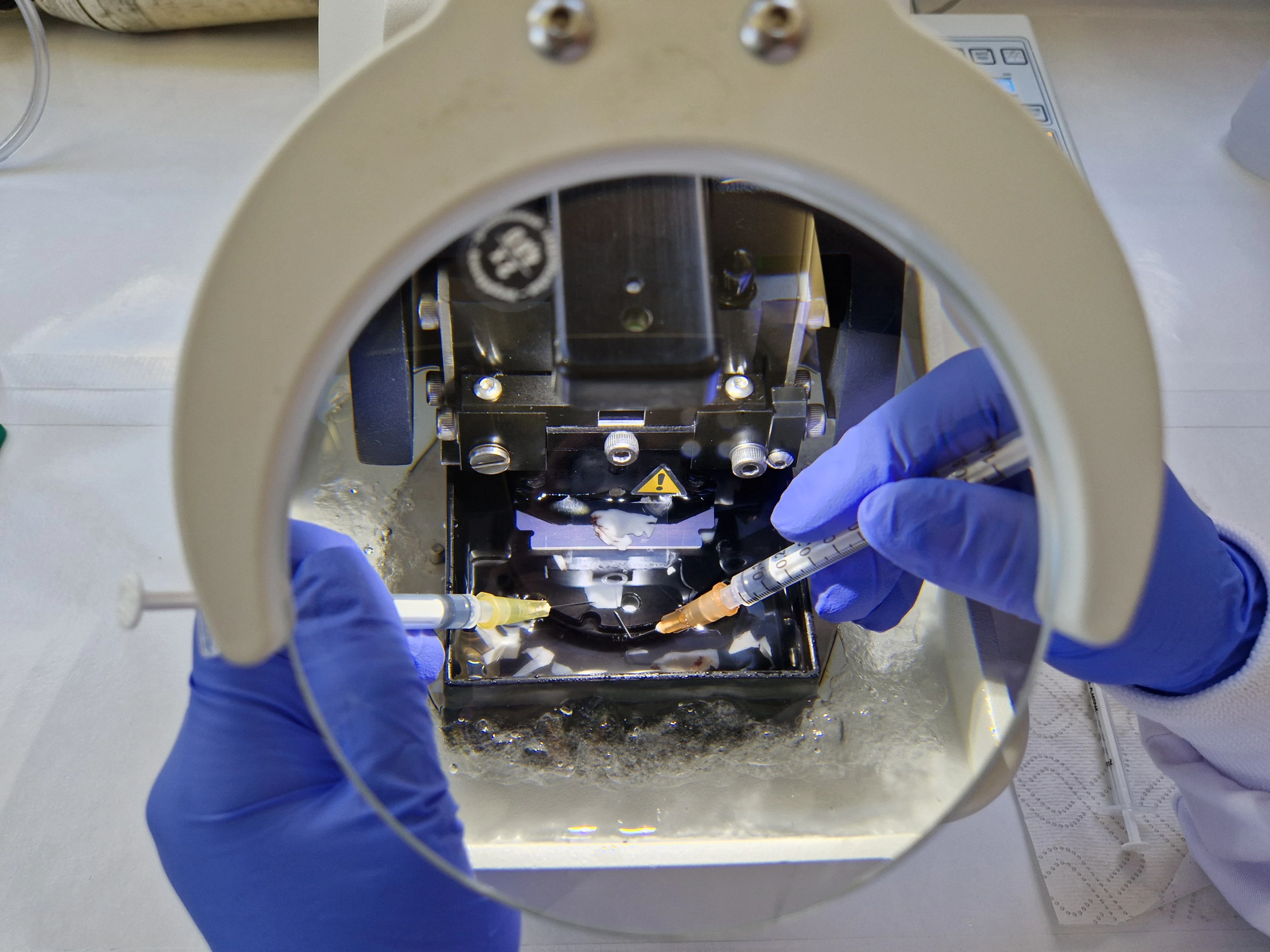
Durrant credits the cross-disciplinary benefits of the RAD Dyson partnership in helping make these findings. The brain tissue she uses in her work is donated by participants who need to have small portions of their brains removed during other surgical procedures. This tissue is then sliced extremely thinly, and examined at the molecular level using technology developed by Dyson.

“So far, I’ve designed my experiments using equipment available in my lab," she said. "But working with Dyson, I’m asked questions about my methodology and apparatus that I’d never considered. People haven’t thought of working in this way because biology and engineering are two disciplines that normally sit on parallel tramlines. I can’t think of any other science scheme where you get access to different people and game-changing resources in the same way that you do in the Race Against Dementia Dyson Fellowship; it’s really phenomenal.”
The novel use of living tissue, say fellow collaborators, will allow more accurate development of dementia treatments as it can sidestep the use of animal models and speed up clinical trials of potentially life-and-cognition-saving drugs.
"I’ve been delighted to support Dr. Durrant's novel approach," said James Dyson, founder of Dyson. "Working with brain surgeons and their consenting patients nationwide to collect samples of living human brain and keep them alive in the lab is a groundbreaking method. It allows researchers to better examine Alzheimer's disease on real human brain cells rather than relying on animal substitutes, such as mice. Dr. Durrant’s findings show that she is progressing towards solving one of the most devastating problems of our time."
You can hear more from Durrant, Dyson, and Stewart in the following video about the RAD Dyson Fellowship initiative.
Sources: The University of Edinburgh, Dyson