Water-based exercise not only improved muscle strength in people with chronic low back pain, but it also improved quality of life, according to a new study. Aquatic therapy could be a viable alternative for those who fear moving or exercising due to pain.
Chronic low back pain (LBP) can be debilitating because of its ability to impact important areas of daily life: mobility, work, sleep, and mental well-being. It’s why there’s been so much research into what treatments effectively relieve the condition, and those that are less effective.
New research by Canada’s Concordia University has tested the effectiveness of aquatic exercise in reducing pain and improving function in people with chronic LBP and found that it does more than just strengthen back muscles.
“Getting into water makes people feel better right away, because it takes away loading on the spine,” said Maryse Fortin, the study’s corresponding author and an associate professor in Concordia’s Department of Health, Kinesiology and Applied Physiology. “This made aquatic therapy an interesting medium to study people who have pain-related fear, like kinesiophobia (the fear of movement stemming from a fear of pain or injury) and pain catastrophizing, and how those relate to spinal musculature.”
The researchers recruited 34 adults who’d had chronic, nonspecific LBP for more than three months and randomly divided them into two groups. The SwimEx group did aquatic exercises designed to engage the deep trunk muscles twice a week for 10 weeks. The standard care group received typical land-based therapy, including stretching, strengthening, and aerobic conditioning. At baseline and after the 10-week intervention, participants self-reported on pain, disability, quality of life, anxiety, depression, sleep quality, and fear of movement. They also underwent lumbar muscle strength testing and MRI scans to assess muscle size and fat content.
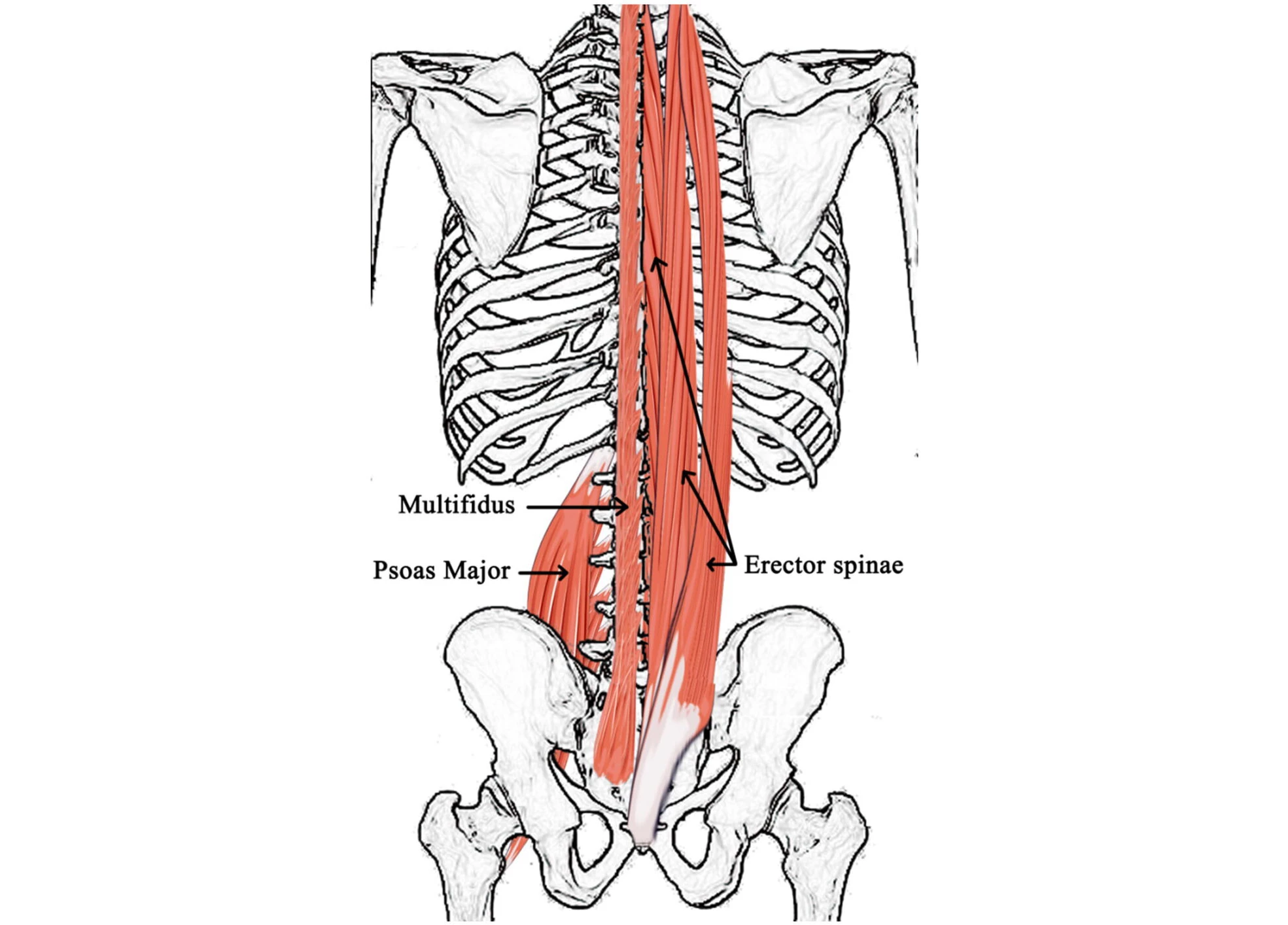
Participants in the SwimEx group showed small but significant increases in the size of the multifidus (MF) and erector spinae (ES) muscles, two sets of upper spinal muscles that support and stabilize the spine, at the lumbar level. Both groups showed improved back strength. While the SwimEx group had a slightly better increase in maximum strength, the standard care group showed slightly better improvement in average strength, possibly because they started with better function.

Regarding participants’ self-reported symptoms, the researchers observed that increases in MF muscle size were moderately associated with better physical quality of life, lower anxiety and depression, and improved sleep quality. However, they saw no clear link between muscle changes and strength gains, suggesting that strength improvements might come from better motor control or coordination rather than just bigger muscles.
The study provides scientific support that water-based exercises can safely and effectively improve muscle size and back strength in people with chronic LBP. The findings are especially helpful for people who are afraid of pain or reinjuring themselves while doing land-based exercises. Furthermore, even small improvements in muscle health were associated with reduced anxiety, improved mood, and enhanced sleep, factors that are often overlooked in traditional LBP treatment but are crucial for long-term recovery.
“Combined with the reduction in anxiety, pain-based fears and sleep disturbances, these make for really interesting findings, and we definitely need to look at the relationship more closely,” Fortin said. “The changes were clinically significant, not just statistically significant, meaning they have a true impact on how the participants feel.”
Because chronic LBP is complex and differs from person to person, this study supports the idea that personalized treatments like aquatic therapy can be very beneficial for people with pain-related fear or poor mobility.
The study was published in the journal Scientific Reports.
Source: Concordia University