A protein notorious for its role in Alzheimer’s disease may hold the key to supercharging the aging immune system, according to new research. Scientists have found that a byproduct of amyloid-beta rejuvenates T cells, boosting their tumor-fighting power and dramatically reducing cancer risk.
As has been seen with some other health conditions, such as obesity, there exists a paradox between cancer and Alzheimer’s disease. That is, research has repeatedly shown that people with Alzheimer’s disease are less likely to develop cancer.
Now, in a new study by the Hollings Cancer Center at the Medical University of South Carolina (MUSC), researchers have uncovered what drives this paradoxical relationship.
“What we found is that the same amyloid peptide that is harmful for neurons in Alzheimer’s is actually beneficial for T cells in the immune system,” said Besim Ogretmen, PhD, associate director of Basic Science at Hollings, and the study’s corresponding author. “It rejuvenates the T cells, making them more protective against tumors.”
The protein amyloid-beta (Aβ) has been associated with Alzheimer’s disease for nearly 40 years and has driven the development of therapies that target the pathological hallmarks of Aβ plaques seen in the disease. In the present study, five years of nationally representative surveys were analyzed, and the researchers found that adults over 59 with Alzheimer’s disease were a staggering 21 times less likely to develop cancer than those without the disease. They then set about understanding why.
The researchers focused on a protein called amyloid-beta precursor protein (APP), a molecule strongly linked to Alzheimer’s, and how APP and one of its breakdown products, amyloid-β 40, behave inside T cells, a type of immune cell that attacks tumors. As T cells age, they can overactivate a process called mitophagy, their mitochondrial “clean up” process, leading to excessive mitochondrial loss and weaker immune responses. This leads to T cells with a reduced cancer-fighting ability.
To get to the “why,” the researchers conducted various experiments on human and animal cells and live animals. They used genetically modified mice with Alzheimer’s-like features and compared them to non-Alzheimer’s mice. Then they implanted these mice with cancer cells to see how fast tumors grew. They took T cells from Alzheimer’s mice and transferred them into non-Alzheimer’s mice with cancer to see if the immune cells alone could slow tumor growth. They also studied how mitophagy behaved in T cells. And they measured changes in key molecules like fumarate, a metabolite vital for energy and mitochondrial function, and proteins like Parkin, which is involved in tagging damaged mitochondria for destruction. The researchers then added extra fumarate or healthy mitochondria to T cells to see if that could reproduce the cancer-fighting effects seen in Alzheimer’s cells.
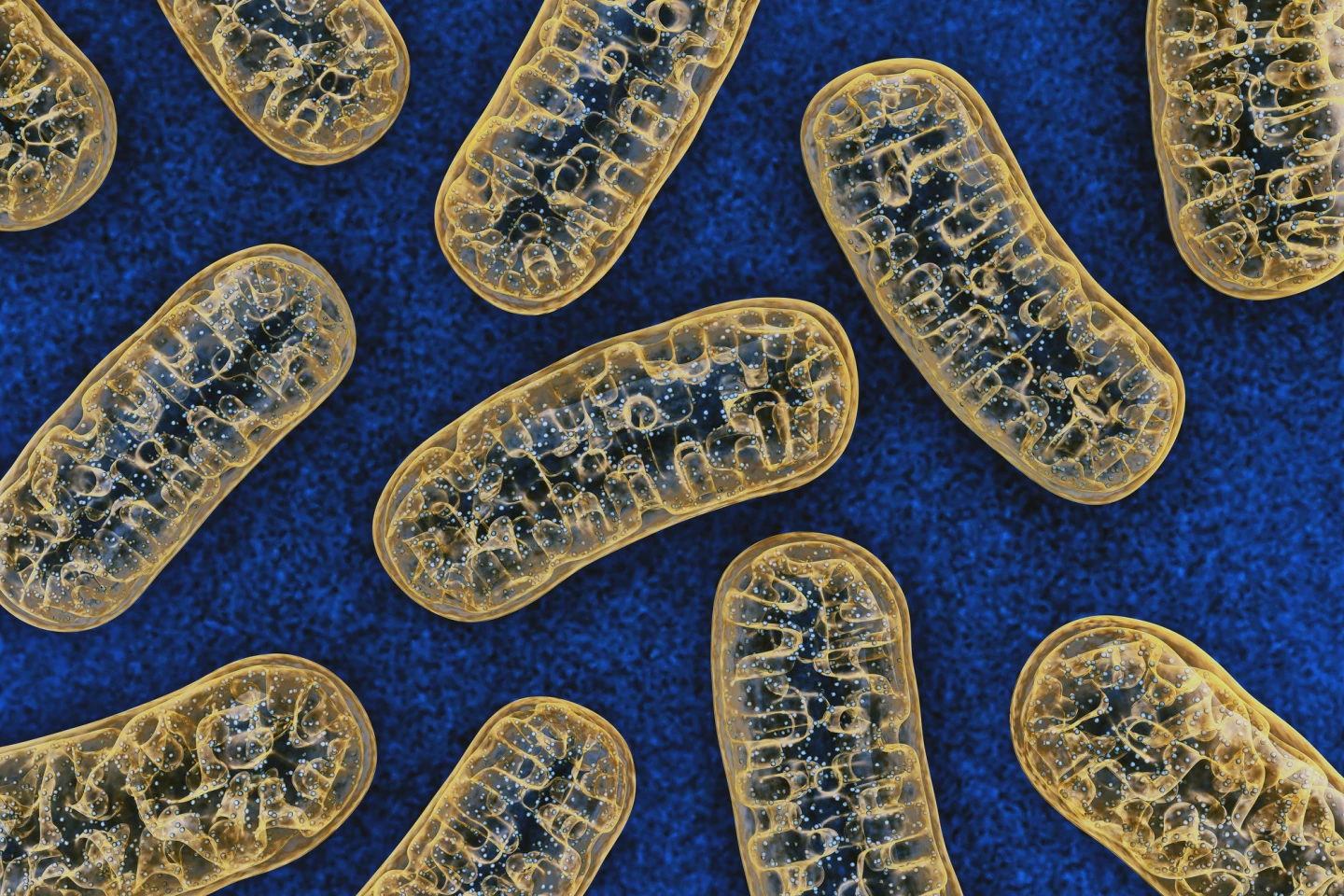
They found that in Alzheimer’s mice, APP and its amyloid-β 40 fragment moved into mitochondria and blocked overactive mitophagy, which kept the T cells healthier and more functional. Cancers grew much more slowly in Alzheimer’s mice; even transferring T cells from Alzheimer’s mice into non-Alzheimer’s mice made tumors shrink, showing that the effect was immune-driven, not just due to Alzheimer’s factors.
Aging T cells typically lose fumarate, which disrupts the chemical modification (“succination”) of Parkin, accelerating mitochondrial damage and mitophagy. APP prevented fumarate loss, protecting mitochondria and improving T cell function. It also interfered with the movement of a protein (CerS6) that produces ceramide, a lipid that triggers mitophagy. This blockage stopped the harmful mitophagy cycle in T cells.
“When you deplete fumarate, you increase mitophagy much more,” Ogretmen said. “Fumarate no longer binds proteins involved in that process, so the proteins become more active and induce more mitophagy. It’s like a reinforcing feedback loop.”
However, giving aging T cells extra fumarate or healthy mitochondria produced the same cancer-fighting boost as APP, highlighting a potential therapeutic strategy.
T cells from older humans showed the same pattern: too much mitophagy and low fumarate. But in T cells from older people with Alzheimer’s, these problems had been corrected, just as they had in mouse models.
“Older T cells began functioning like young, active T cells again,” Ogretmen said. “That was an incredible finding because it suggests a whole new way to think about rejuvenating the immune system.”
Taken together, these findings offer a powerful explanation for why people with Alzheimer’s are less likely to get cancer. It also opens up new therapeutic ideas. Targeting mitophagy, restoring fumarate, or modulating APP-related biological pathways could be ways to reinvigorate aging immune cells, potentially improving cancer immunotherapy in older adults.
The study was published in the journal Cancer Research.
Source: MUSC Hollings Cancer Center






