For the first time, researchers have identified a protein that represses the activity of energy-burning brown fat. The discovery opens the door to developing treatments for the extreme weight loss, muscle wasting, and malnutrition seen in some types of cancer.
Most research into energy-burning brown fat, also known as brown adipose tissue (BAT), has focused on finding ways to activate it, converting "bad" white fat to "good" brown fat to reap the associated health benefits.
Now, a new study led by researchers from the University of Barcelona (UB) in Spain has identified a protein molecule that represses the activation of BAT, and could be valuable for treating the malnutrition, weight loss and muscle wastage associated with some cancers.
“Although the problem is to know what reduces the activity of brown fat, until now, research has focused on identifying the factors that activate its function in the organism, but not the factors with a repressive function,” said corresponding author Professor Francesc Villarroya, from UB’s Faculty of Biology. “As a result, it was generally assumed that the low activity of brown fat in aging and obesity could be explained by the fact that its activators do not work properly.”
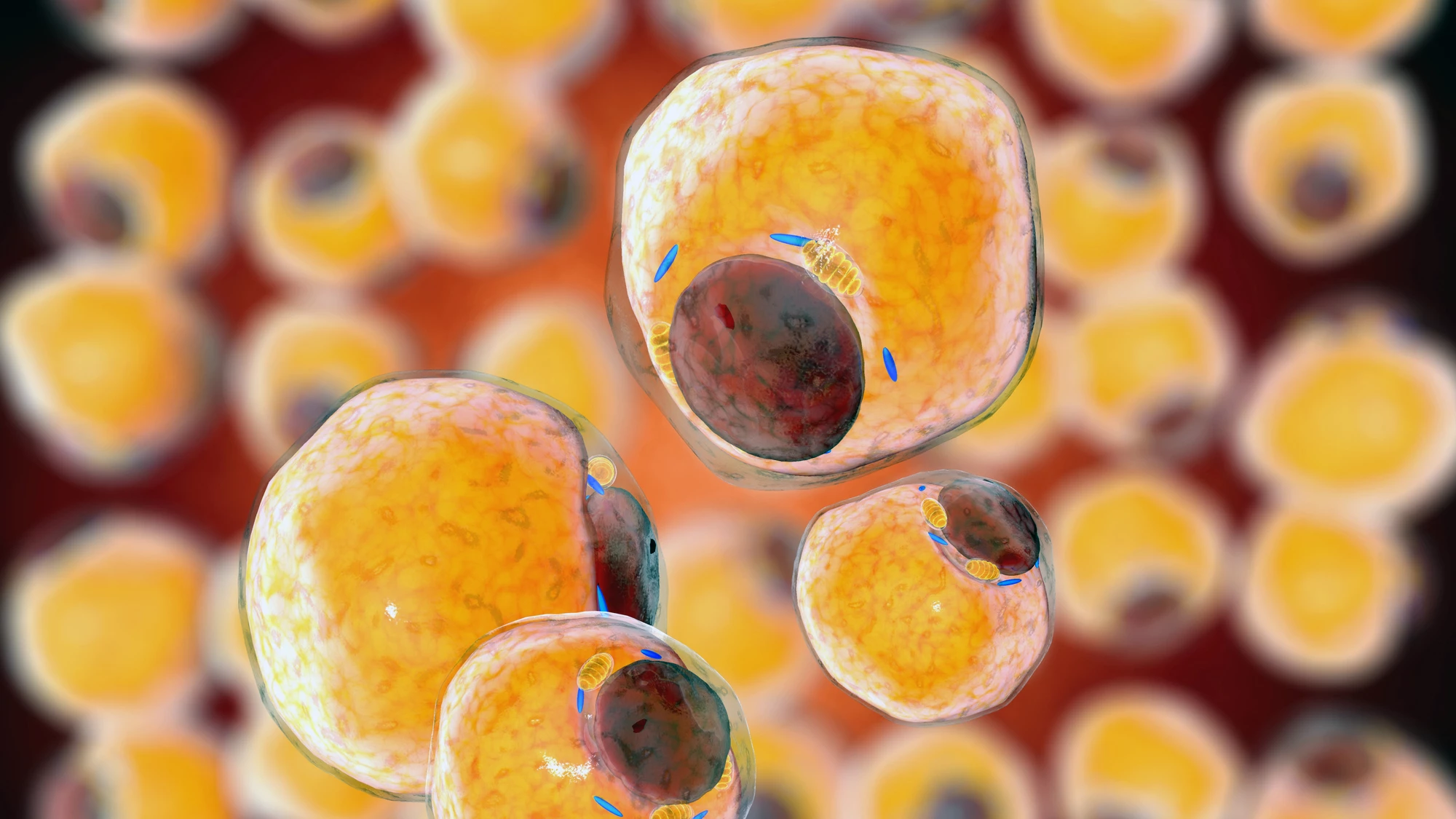
The function of white fat, or white adipose tissue (WAT), is primarily to store energy. It stores excess energy from food in the form of fat and releases it when needed, also providing insulation and cushioning. When WAT accumulates beyond what the body needs for energy storage, it can lead to obesity. BAT, on the other hand, burns fat and generates heat to maintain body temperature, a process called thermogenesis. Its brownish color is attributable to the large number of mitochondria, the cells’ energy-producing machinery. BAT can be activated to burn calories and produce heat when needed, such as in cold conditions.
In the present research, the researchers discovered for the first time that a particular protein, acyl CoA-binding protein (ACBP), acts like a brake on BAT’s thermogenesis. When lab cell cultures were given extra ACBP, their ability to burn fat and generate heat was reduced. The researchers then created mice with the ACBP gene removed only in brown fat cells and exposed the animals to cold and high-fat diets to see how their BAT responded. The ACBP-less mice had higher BAT activity, produced more heat, had smaller fat stores, better blood sugar control, and gained less weight despite eating a high-fat diet. The findings suggest that ACBP acts like a brown fat regulator, telling it to “cool it” when it’s been active for a while.
While a high level of BAT activity is generally associated with a healthy metabolism, overactivation of BAT may become pathological in some cancers and in patients with severe burns. In these situations, BAT overactivation can lead to a complex metabolic disturbance known as cachexia, where the body breaks down muscle and fat at an accelerated rate, often despite adequate nutrition. It leads to unintentional weight loss, muscle loss, and overall tissue wasting that significantly impairs physical health and quality of life. Identifying the role of ACBP might lead to therapeutics to assist cachexic patients.
“In some cancers, brown adipose tissue becomes pathologically overactive and causes uncontrolled metabolic energy expenditure, leading to cachexia,” Villarroya said. “In this case, the function of the ACBP protein as a repressor factor could become a therapeutic tool of interest in cancer patients.”
Additionally, studies have shown that warmer ambient temperatures, such as those seen with global warming, can decrease the amount of BAT or make it less active, contributing to obesity. The researchers say ACBP may be playing a role here, too.
“An excess action of the ACBP protein blocking the activity of brown fat would be the molecular basis of this phenomenon,” said Villarroya. “Once this factor has been identified, we can design intervention tools to promote a healthier lifestyle.”
The study was published in the journal Molecular Metabolism.
Source: University of Barcelona