Is obesity a disease or a risk factor for disease? In medical circles – and outside of them – the question is contentious, with supporters on either side. In a newly published report, the Global Commission on Clinical Obesity has strived to settle the debate, introducing a new framework that redefines obesity.
“The question of whether obesity is a disease is flawed because it presumes an implausible all-or-nothing scenario where obesity is either always a disease or never a disease,” said Professor Francesco Rubino, Commission Chair, Chair of Metabolic and Bariatric Surgery at King’s College London. “Evidence, however, shows a more nuanced reality. Some individuals with obesity can maintain normal organs’ function and overall health, even long term, whereas others display signs and symptoms of severe illness here and now.”
In addition to consulting with people living with obesity, the Commission involved 56 world-leading experts from different countries with diverse healthcare systems. They came from various medical specialties, including endocrinology, internal medicine, surgery, biology, nutrition, and public health.
Obesity: Disease or risk factor? (And why it matters)
Obesity has been a known risk to health since Hippocrates’ time. Indeed, the Greek physician and teacher wrote about the dangers of eating ‘more food than the constitution will bear.’ And (probably) since then, there has been disagreement about whether obesity is a risk factor for disease or a disease in its own right.
“The reason why it has never been settled is because obesity is a spectrum,” Rubino explained. “And this idea of only a disease or only a risk factor really clashes with a reality where you can have people who have normal – preserved, normal – organ function and can go about their lives for quite some time in a pretty normal way, sometimes even for a lifetime.
“But on the other hand, there are people who have excess body fat, and not because of other diseases that are associated with obesity, but because of excess body fat itself,” he continued. “They experience impairment in the functions of their organs – the heart, the joints, the kidneys, the liver, and so on – so that substantially, we have the typical manifestations of an ongoing illness. So there are some people who have a disease here and now because of obesity, but there are others that have relatively preserved, good function of their organs and still have obesity.”
Does it matter how obesity is defined? Yes. Because of the way it’s currently defined and measured, obesity doesn’t have the same meaning for all individuals with the condition. It’s arguable, then, that there are benefits to adopting a uniform approach, one that ‘picks a side’ in the longstanding disease-versus-risk factor debate. For one, recognizing obesity as a disease acknowledges the contribution made by genetics and environment, shifting the blame away from ‘poor personal choices,’ which could reduce the stigma of seeking treatment for the condition. Additionally, disease classification may improve access to healthcare, promote insurance coverage for treatment, and prioritize funding for obesity research.
The Commission has ostensibly settled this disagreement by opting to classify obesity as a disease and developing a new framework that included a more nuanced definition that put obesity on equal footing with other chronic illnesses and could guide the management and treatment of the condition.
“Such reframing can provide a crucial, missing piece in the way we conceptualize and approach obesity, with important ramifications for clinical practice, public health policies, and societal views of obesity,” the commissioners said in their report. “This Commission was established to identify clinical and biological criteria for the diagnosis of clinical obesity that, akin to diagnostic methods for chronic diseases in other medical specialties, reflect ongoing illness.”
Why BMI alone is not great for diagnosing obesity
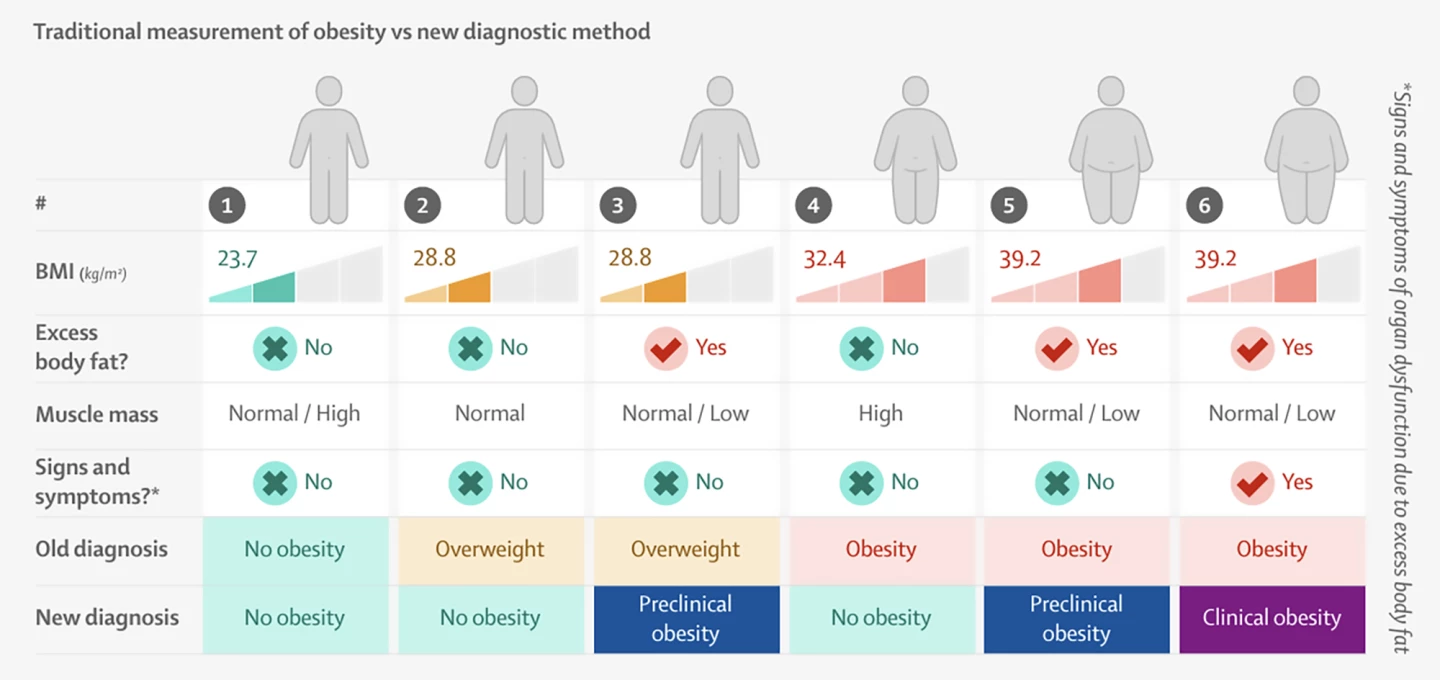
BMI is an internationally recognized standard for assessing whether individuals are a ‘healthy’ weight. It’s calculated by dividing body mass by the square of body height, resulting in a figure expressed in units of kg/m2. As a screening measure, BMI is a quick, cheap, and reliable measure of categorizing someone as underweight (less than 18.5 kg/m2), a healthy weight (18.5 to less than 25), overweight (25 to less than 30), or obese (30 or greater).

However, when it comes to diagnosing obesity, BMI can be a somewhat blunt, imprecise instrument. It doesn’t distinguish between fat, muscle, and bone mass, which can influence a person’s weight. Nor does it indicate what types of fat people are carrying, where on the body they’re carrying it, whether there is organ or tissue dysfunction, or an inability of a person to conduct normal everyday activities. It follows that, if used alone, BMI could result in the overdiagnosis of obesity in otherwise healthy individuals.
“Body mass index only takes into account body weight and the height of an individual,” Rubino said. “So, of course, it doesn’t compute the body composition. It doesn’t tell us, in fact, if there is an elevated BMI due to excess body fat. So, BMI may actually be failing some individuals, at least, to even detect the very condition that we call obesity, in other words, excess body fat. Body mass index doesn’t tell us how well our organs are working, if they’re still normal or they’re … dysfunctional and, therefore, whether there is health or illness at the individual level. So, this classification doesn’t help.”
To reduce the risk of misclassification, the Commission’s strong view was that it was more appropriate to assess the effect of excess fat on health by considering abnormalities in the mass, distribution and function of adipose tissue rather than relying on BMI alone. They recommended that, as with other chronic diseases, the diagnosis of obesity by medical professionals should be based on an assessment that includes confirming excess body fat by one of the following methods:
- at least one measurement of body size (waist circumference, waist-to-hip ratio, or waist-to-height ratio) in addition to BMI;
- at least two measurements of body size (waist circumference, waist-to-hip ratio, or waist-to-height ratio) regardless of BMI;
- direct body fat measurement, such as by bone density scan (DEXA), regardless of BMI;
- in people with a very high BMI – for example, higher than 40 kg/m2 – excess body fat can be pragmatically assumed.
In addition, the new diagnostic model relies on objective assessment of illness at the individual level, including measuring blood biomarkers for organ and tissue function and assessing how well a person performs activities of daily living like bathing, dressing, toileting, and eating.
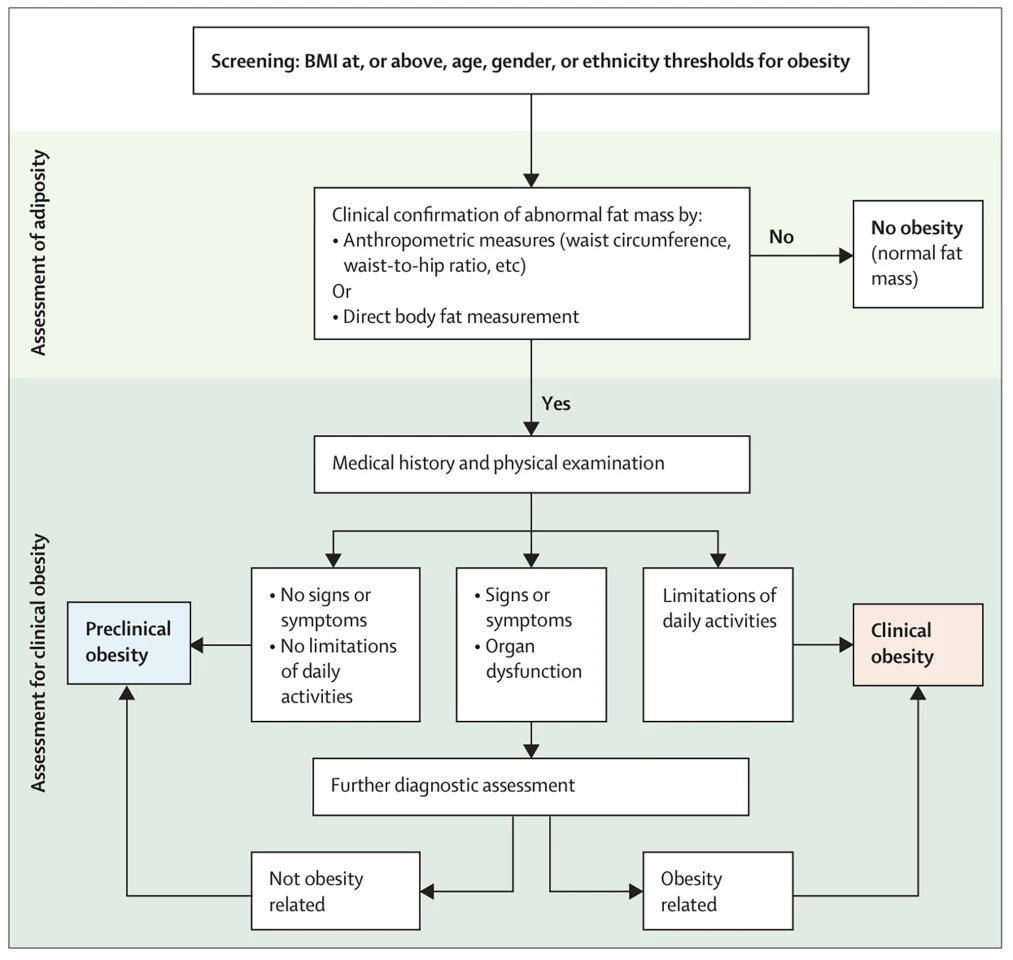
“The question is, is whether that excess body fat is actually creating any problems in terms of obesity-related organ dysfunction, or limitations of daily activities, or both,” said Commissioner Louise Baur, Professor of Child and Adolescent Health at The University of Sydney, immediate past President of the World Obesity Federation. “If not, if the person is otherwise well, then we call that ‘preclinical obesity.’ But if the person does have these other health issues, then we call that ‘clinical obesity.’”
The new framework: Introducing clinical and preclinical obesity
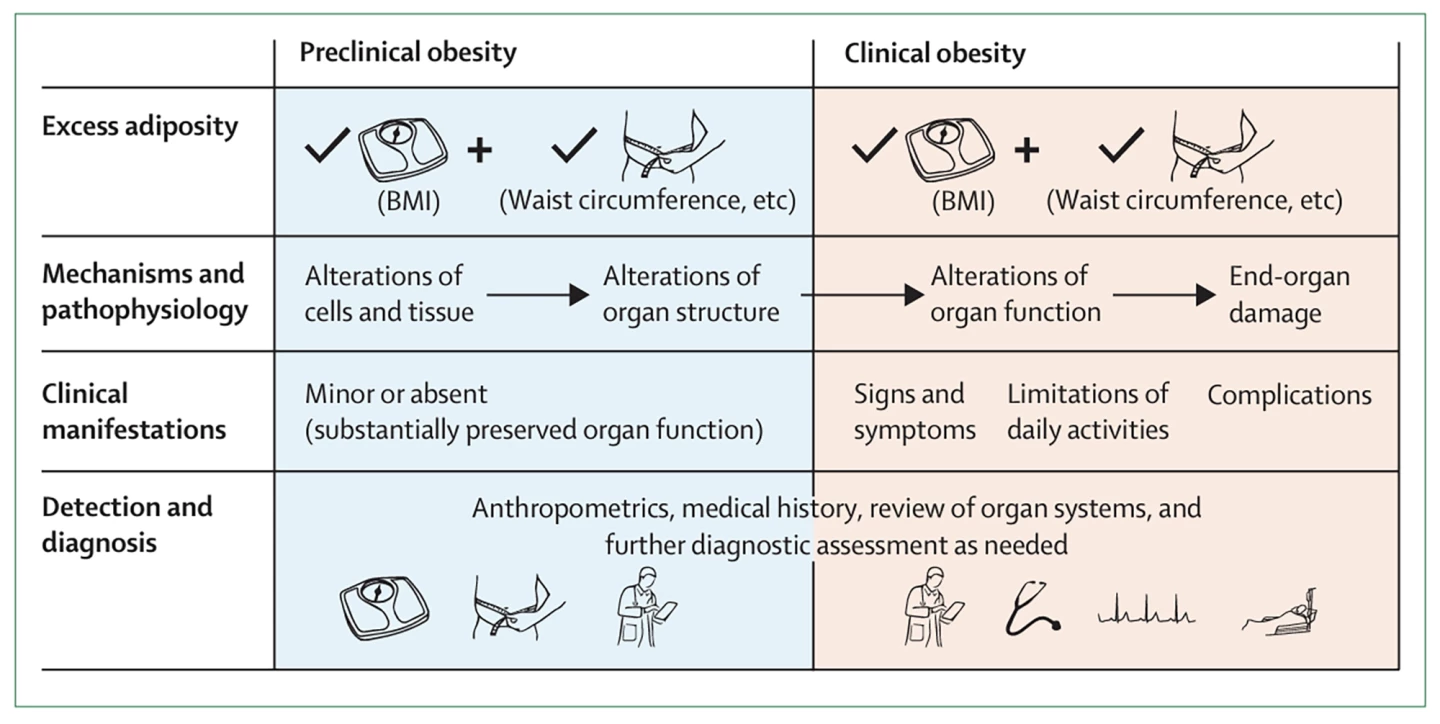
Based on the holistic assessment discussed above, under the Commission’s framework, a person is diagnosed with clinical or preclinical obesity. Clinical obesity is defined as a chronic illness resulting from organ or whole-body dysfunction that is directly caused by excess fat, independent of the presence of other adipose-related diseases. Preclinical obesity is a condition of obesity with normal organ function.
“We’ve introduced the concept of clinical obesity as a distinct and standalone disease, not something that really reflects other diseases, and it recognizes that obesity can co-exist with preserved organ and whole-body function,” Baur said, highlighting how the framework differentiates between individuals with preserved health and those who have illness due to obesity alone.
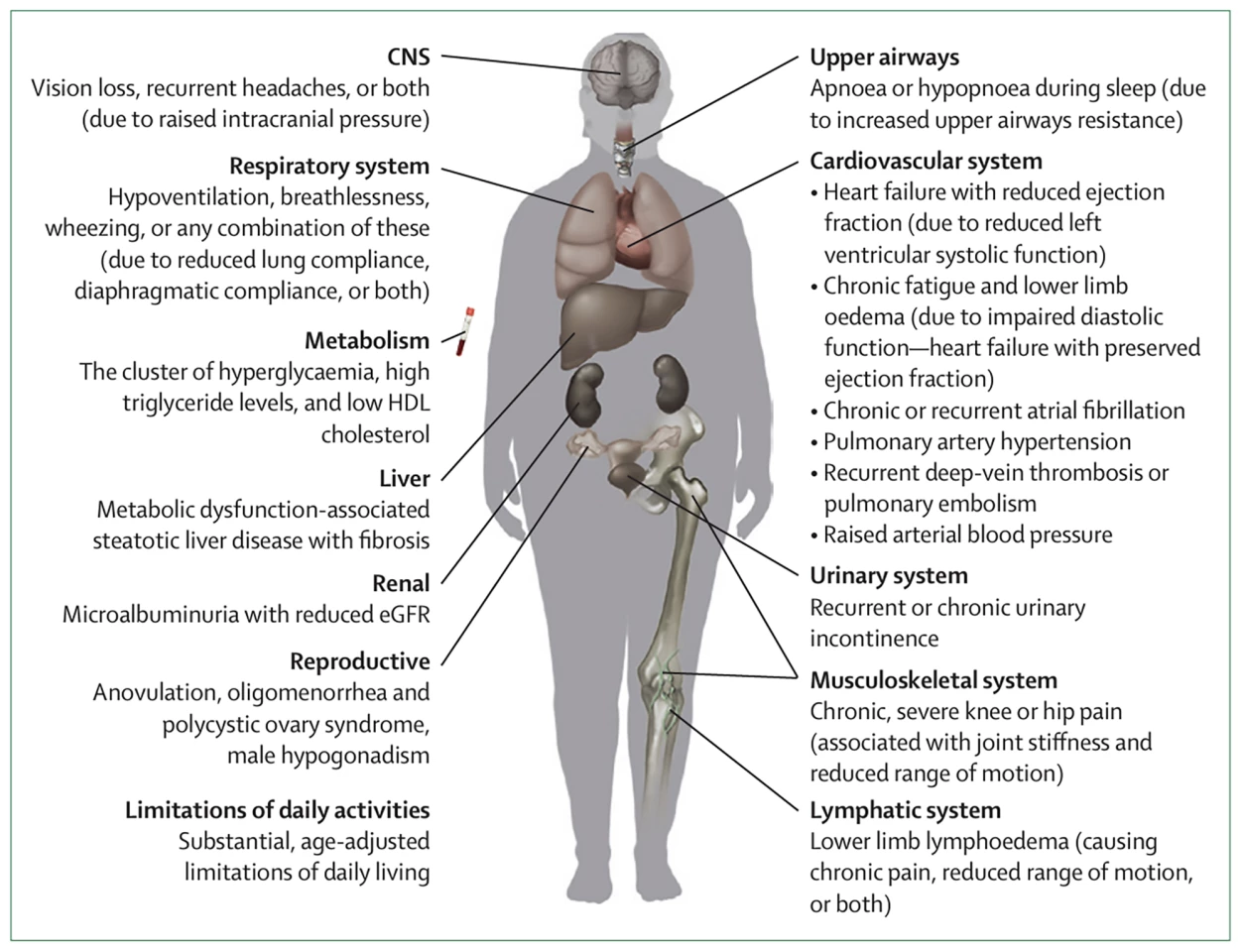
The framework sets out 18 diagnostic criteria for clinical obesity in adults and 13 criteria for children and adolescents. The criteria include things like sleep apnea, high blood glucose levels, chronic, severe knee or hip pain, chronic fatigue, lower limb swelling, chronic headaches and vision loss.
The Commission’s ultimate aim is to ensure that individuals with clinical obesity have timely, equitable access to comprehensive care and treatment appropriate for those with a chronic, potentially life-threatening illness. And for those diagnosed with preclinical obesity to have access to counseling, health screening and monitoring over time, and appropriate care as needed to reduce the risk of the condition developing into clinical obesity and/or other adiposity-related diseases.
“We’ve come up with an objective diagnostic model that allows standardization across the global health system,” said Baur. “So, the whole idea here is that this should be able to work in low- and middle-income countries, as well as in highly resourced, high-income countries.
“Our approach reduces the influence of age and gender and ethnicity on diagnosis and treatment decisions. The concept allows patient-tailored treatment strategies such as risk reduction, particularly in those with preclinical obesity, versus more intensive treatment in those with clinical obesity.”
The years that the commissioners spent exploring obesity – the Commission was approved back in 2021 – to develop this framework exposed crucial knowledge gaps about the cause, pathophysiology, management, and societal effects of obesity, which they hope will be addressed by future research. Until then, they want health professionals to embrace the new approach.
“With the new criteria proposed by the Commission, we finally have a meaningful way of diagnosing obesity, meaning we can tailor the treatment plan according to the patient’s needs,” said Professor Wendy Brown, Commission member and Chair of the Monash University Department of Surgery, School of Translational Medicine at Alfred Health.
The Commission's report was published in The Lancet Diabetes & Endocrinology journal.
Source: The Lancet via Scimex, Monash University










