As more bacteria that cause diseases become increasingly resistant to antibiotics, we need more ways to fight off infections. That's where this new patch comes in. With just a gentle electric zap, this bioelectronic wearable could prevent bacteria from doing a number on us through our skin.
The breakthrough comes from researchers at the University of Chicago and the University of California San Diego. In a paper published in the Device journal this week, the team detailed how the device lowers the activity of harmful genes in infectious bacteria, and curbs their growth.
The study was successfully carried out using a bacterium called Staphylococcus epidermidis on pig skin. That's a commonly occurring bacterium known for causing hospital-acquired infections. If it can target various types of bacteria safely, we could be looking at a novel drug-free treatment for bacterial infections that doesn't give a damn about their resistance to antibiotics.
Through their study, the researchers discovered that some bacteria were “selective” about the environment in which they display excitability, i.e. being reactive to some external stimulus. They found that Staphylococcus epidermidis became electrically excitable under healthy skin, which is an acidic environment.
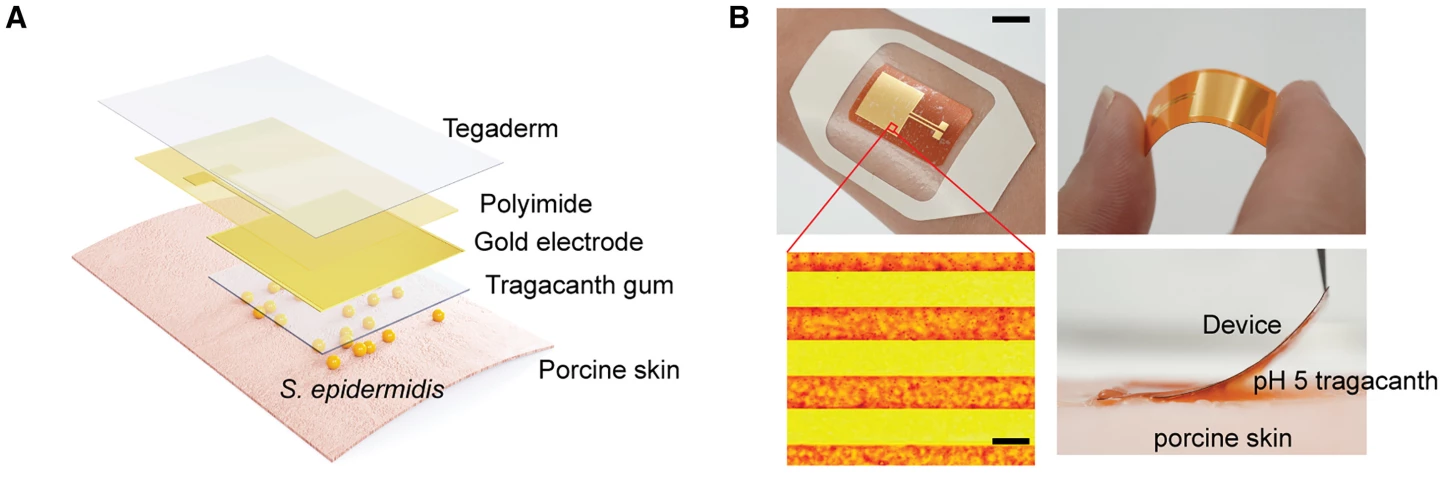
Armed with this knowledge, they set about demonstrating their findings with the bacterium on pig skin using a flexible patch they called Bioelectronic Localized Antimicrobial Stimulation Therapy, or – wait for it – BLAST. They also created an acidic environment on the skin using a hydrogel.
Sending a weak electric signal of 1.5 volts – far lower than the 15-volt safety limit for humans – for 10 seconds every 10 minutes for 18 hours through the patch stopped 99% of the bacteria cluster that forms to block drugs and cause infections. There were also nearly 10 times fewer S. epidermidis cells on the treated skin sample, compared to the untreated sample, after the 18-hour cycle.
This could be a big win for treating infections for a couple more reasons. Beyond working on antibiotic-resistant bacteria, it could negate the need for antibiotics for certain kinds of infections – meaning it could be deployed in remote areas where medicine is difficult to deliver regularly. Plus, the small patch enables targeted treatment on a small area of the skin, and that could reduce the chance of potential side effects.
As you'd expect, there's plenty more work to be done in this field. "Discovering this selective excitability will help us discover how to control other bacteria species by looking at different conditions," noted first author Saehyun Kim from the University of Chicago.
Senior co-author Bozhi Tian, also from the University of Chicago, explained that there's scope to develop a patch with a wireless circuit to control infections without drugs, and further examine the effectiveness of this treatment.
According to the World Health Organization, bacterial antibiotic resistance was directly responsible for 1.27 million deaths around the world in 2019. That means this treatment could potentially help prevent serious conditions that result from antibiotic-resistant bacteria, and save lives in the process.





