For some time now, we've been hearing about prosthetic limbs that are designed to work with amputees' bodies. MIT researchers are taking a different approach, though, with a new type of amputation that facilitates the use of prostheses.
Most movements of the arms and legs involve two joined muscles, one of which stretches while the other contracts. These are known as agonist-antagonist pairs, which the biceps and triceps are a good example of – when a person bends their elbow, the biceps muscle contracts as the triceps muscle stretches. That stretching motion relays sensory feedback information to the brain, helping it to keep track of the arm's position.
In most conventional limb amputations, the joined ends of the paired muscles are cut off, keeping them from properly communicating with one another. As a result, the muscle signals that are sent to the brain are confusing. This means that many amputees end up having to visually watch what their prosthesis is doing, in order to guide its movement.
In the new procedure, called agonist-antagonist myoneural interface (AMI), the severed ends of the paired muscles are joined back together after the amputation itself has occurred. Doing so reconnects their communication system, allowing the brain to better gauge where the missing section of the limb would be in three-dimensional space, if it were still attached.
Following lab rat tests performed in 2017, approximately 25 patients have undergone AMI surgery at the Harvard University-affiliated Brigham and Women’s Hospital. The MIT scientists assessed 15 of those people, each of whom had a single below-the-knee amputation.
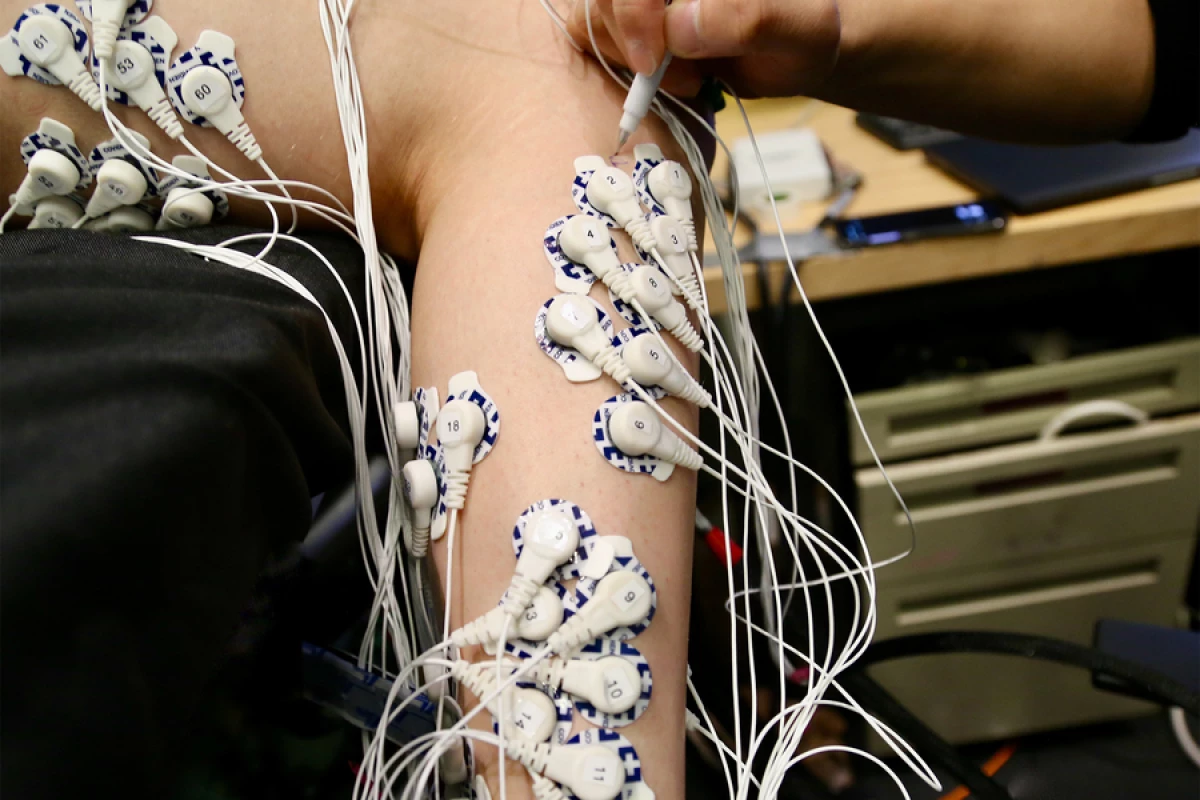
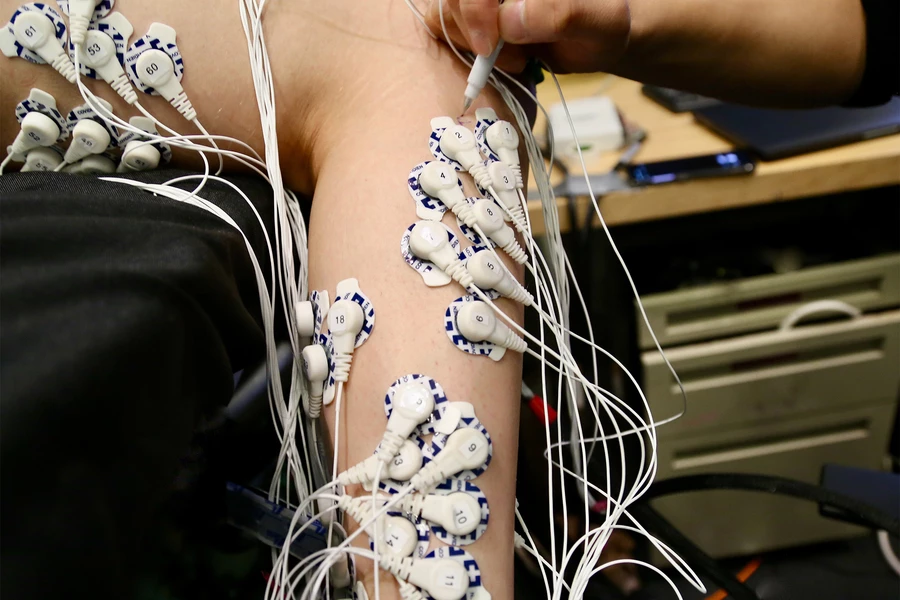
Testing consisted of having the patients lie down with both legs propped up, without a prosthesis in place. They were then asked to flex both their intact ankle joint and that of their "phantom limb" to varying degrees, while electrodes on both legs monitored the electrical activity of the muscles.
As compared to a control group that had received conventional amputations, the AMI amputees were found to have much finer control over their phantom ankle – this was evidenced by the fact that the electrical signals in the stump of their amputated leg were significantly more similar to those in their intact leg, on which the ankle was actually moving.
Likewise, brain scans showed that they were receiving more sensory feedback from their residual muscles. And as a side benefit, the AMI group reported much less pain in their residual limb.
Further studies will be required to see if the benefits of the procedure do in fact result in better control over an actual attached prosthesis. It should also be noted that the scientists have developed a version of the surgery known as "regenerative AMI," in which grafted muscle segments can be used to reconnect agonist-antagonist muscles that were previously severed in traditional amputations.
A paper on the research, which is being led by postdoctoral student Shriya Srinivasan, was recently published in the journal Science Translational Medicine.
Source: MIT