Science is continuing to shine a light on the links between gut bacteria and all kinds of health conditions, ranging from depression, to autoimmune disease, to Alzheimer’s and PTSD. A US research team working to further unravel its secrets has happened upon a specific signature of gut bacterial species, which it found could be used to detect liver fibrosis and cirrhosis with an accuracy of greater than 90 percent.
Disease of the liver is one that can progress from a common and non-serious buildup of excess fat in the organ, known as non-alcoholic fatty liver disease (NAFLD), to the harmful scarring and cell death associated with fibrosis, cirrhosis and possibly cancer. Monitoring the condition as it moves into these dangerous phases is possible through MRIs and biopsies, but these are expensive and invasive, so the team behind the new study has been working on a simpler method.
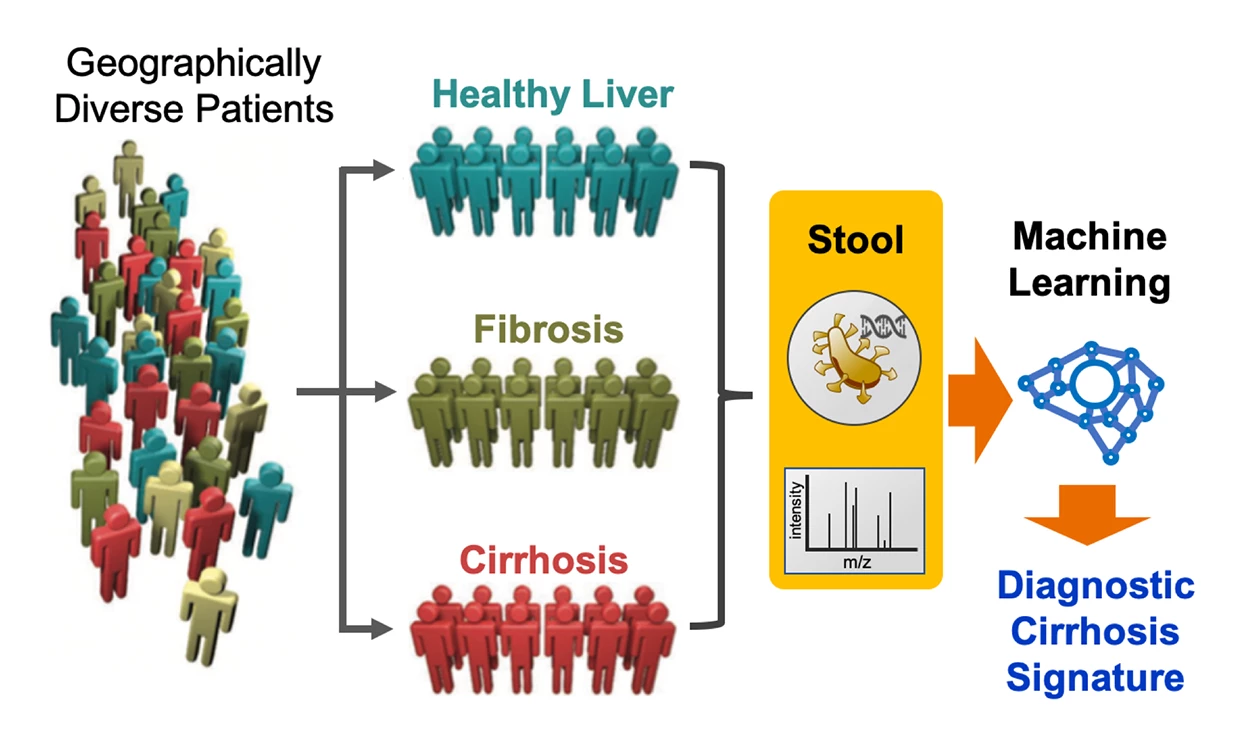
Made up of scientists from the Salk Institute and University of California San Diego, the team explores the relationship between gut bacteria and NAFLD. Its previous work in the area had uncovered links between specific bacterial species and NAFLD in small sample sizes, and it has now expanded the scope of its work and developed a new computational tool to do the heavy lifting.
For its latest study the team enlisted 163 healthy and sick participants, who offered up stool samples for analysis. This involved genetic profiling of the microbiome and examination of the metabolites within the samples, which led to the discovery of a signature based on the presence of 19 bacterial species that was indicative of liver disease.
This set of bacterial species was associated with a cirrhosis diagnosis with an accuracy of 94 percent, and the team says it could also be used to determine the stage of liver fibrosis. With these exciting results, the team then set about verifying the technique on a pair of independent patient groups in China and Italy. Here it again proved highly accurate, correctly identifying cirrhosis in more than 90 percent of patients.
“It is remarkable that a gut microbiome signature derived from patients residing in Southern California for cirrhosis was able to predict cirrhosis in two independent cohorts residing in China and Italy. It speaks to the new discoveries that are yet to be realized in the role of the gut microbiome to diagnose and risk-stratify liver disease,” says Rohit Loomba, co-corresponding author and director of the NAFLD Research Center at the UC San Diego School of Medicine. “I think the power of using the microbiome as a diagnostic tool is only starting to be realized.”
For their next steps, the researchers will investigate whether altering the makeup of the gut bacteria can treat the disease or possibly make it worse, which will help uncover the potential for causal links.
“The microbiome is a dynamic living sensor of small changes in health and disease in the body, and as such, it provides an accurate readout of body health,” says Salk Professor Ronald Evans, co-corresponding author. “Because this diagnostic is fast and low-cost, it could be something that becomes widely used, especially in the many areas that lack specialty clinics and physicians. Simply said, it could be a real game changer, with world-wide implications.”
The research was published in the journal Cell Metabolism.