In what is being described as a world-first, scientists in Israel have reportedly grown spinal cord implants utilizing tissue extracted from human volunteers. Those implants were then used to restore full walking abilities to previously paralyzed mice.
The research is being led by Prof. Tal Dvir, at Tel Aviv University's Sagol Center for Regenerative Biotechnology. His team started by taking small samples of belly fat tissue from three people, then separating the somatic cells within that tissue from the extracellular matrix material that surrounded them.
A genetic engineering process was then used to reprogram the cells, reverting them to what are known as induced pluripotent stem cells. The extracellular matrix, meanwhile, was converted into a hydrogel. Because the gel was made from each person's own tissue, that means it wouldn't be rejected by their immune system if it were to be implanted into their body.
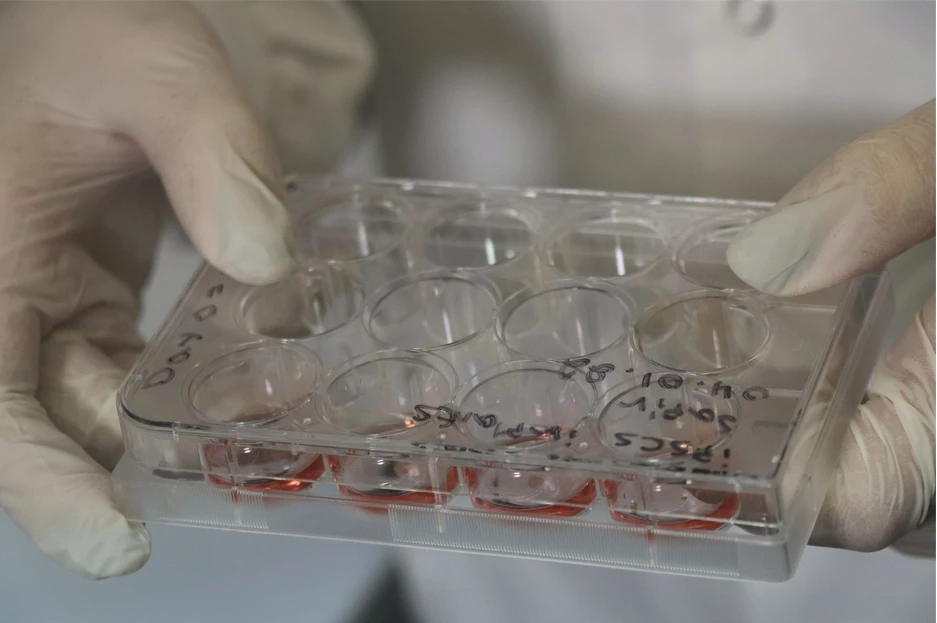
The stem cells were subsequently encapsulated within the hydrogel, via "a process that mimics the embryonic development of the spinal cord." After 30 days, the result was a batch of three-dimensional spinal cord implants, each one made up of neuronal networks that contained motor neurons.
Those implants were subsequently implanted into mice that had lost the use of their left hind leg due to a partially severed spinal cord.
In one group – that had just recently been injured – the implant successfully bridged the gap in their spinal cord, allowing 100 percent of the mice to regain full use of the leg after a rehabilitation process. In another group, which had been injured six weeks earlier, the success rate was still around 80 percent – in that case, scar tissue which had formed at the injury site had to be removed before the implant was put in place.
The technology is now being further developed via spinoff company Matricelf.
"We hope to reach the stage of clinical trials in humans within the next few years," says Dvir. "Since we are proposing an advanced technology in regenerative medicine, and since at present there is no alternative for paralyzed patients, we have good reason to expect relatively rapid approval of our technology."
A paper on the research was recently published in the journal Advanced Science.
Source: Tel-Aviv University
UPDATE (Feb. 8/22): Responding to a query we sent earlier, one of Prof. Dvir's PhD students has informed us that while human somatic cells were indeed harvested and used in the study, various limitations required the scientists to make the hydrogel out of the extracellular matrix from pig belly fat. Needless to say, in the proposed clinical version of the technology, both the cells and the extracellular matrix would be obtained from the human patient.




