Advances in electronics, sensor technology and wireless communications are converging to open up some exciting possibilities in monitoring the human body from the inside, from sensors that track the status of orthopedic implants to gas-detecting devices that dissolve once their job is done. Engineers at the University of California (UC), Berkeley have demonstrated a new form of this technology that can be used to detect oxygen levels in deep tissues, with hopes it could become a tool to track the health of transplanted organs, among other applications.
The tiny wireless implant was developed to fill a hole in current methods for measuring oxygenation of tissues within the body, some of which involve the use of electromagnetic waves to gather information but can only penetrate a few centimeters beneath the skin. Magnetic resonance imaging is another way to measure deep tissue oxygenation, but takes some time to perform and is unable to offer results in real time.
Smaller than a typical ladybug, the team's new implant actually builds on an earlier creation called "neural dust," which is a tiny wireless implant the size of a grain of sand and can track nerve signals and muscle activity in real time. It does so by detecting voltage spikes in the electrical activity of nerves and relaying that to an external device via ultrasound. A more recent version, dubbed StimDust, is able to actually stimulate the nerves as a potential treatment for chronic pain and epilepsy.

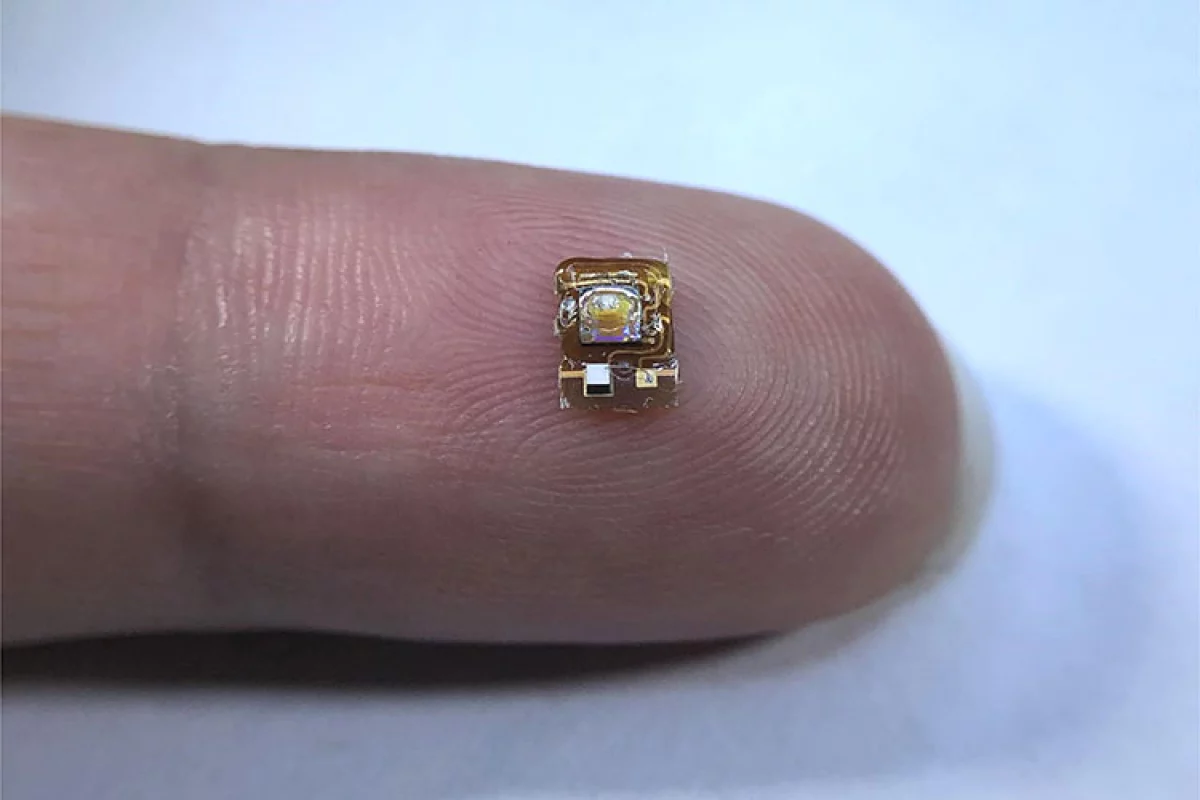
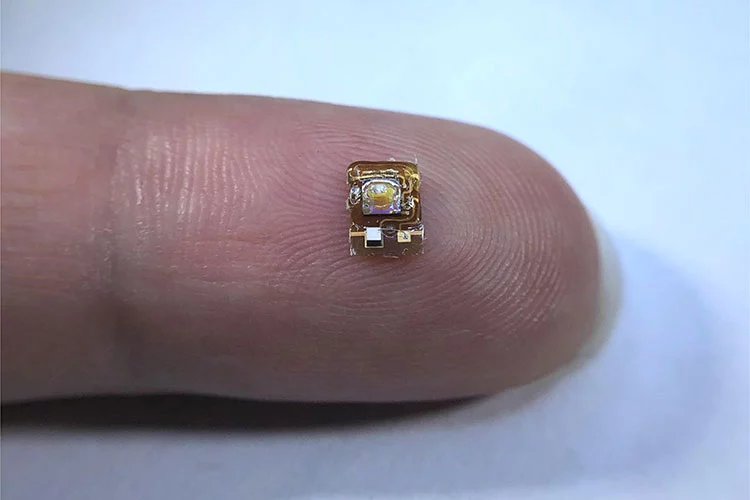
The new implant measures 4.5 mm long and 3 mm wide and incorporates an oxygen-sensing film, a microLED and an optical filter, which work together to measure oxygenation levels in surrounding tissue. This sensor is controlled via an integrated circuit that outputs an electronic signal that varies based on oxygenation levels. A piezo-crystal converts these electronic signals into ultrasonic waves that are then transmitted through the living tissue to an external device.
“It’s very difficult to measure things deep inside the body,” says Michel Maharbiz, a professor of electrical engineering and computer sciences at UC Berkeley. “The device demonstrates how, using ultrasound technology coupled with very clever integrated circuit design, you can create sophisticated implants that go very deep into tissue to take data from organs.”
The authors of the study demonstrated the device in live sheep and see it holding potential in pediatric care, where premature infants could be implanted with it to ensure they are being administered the correct amount of supplemental oxygen. Other possibilities include monitoring the health of transplanted organs, and even improving cancer treatments.
“One potential application of this device is to monitor organ transplants, because in the months after organ transplantation, vascular complications can occur, and these complications may lead to graft dysfunction,” says study author Soner Sonmezoglu. “It could be used to measure tumor hypoxia, as well, which can help doctors guide cancer radiation therapy.”
The scientists hope to improve on the device further by both enabling it to survive long term in the body and also making it smaller, which would make implantation simpler. Other possibilities include tweaking the sensor design to track other biochemistry in the body.
“By just changing this platform that we built for the oxygen sensor, you can modify the device to measure, for example, pH, reactive oxygen species, glucose or carbon dioxide,” Sonmezoglu says. “Also, if we could modify the packaging to make it smaller, you could imagine being able to inject into the body with a needle, or through laparoscopic surgery, making the implantation even easier.”
The research was published in the journal Nature Biotechnology.