A new study has revealed how the mutated proteins that are a hallmark of Parkinson’s disease spread and aggregate in the brain. The finding opens the door to developing a way of halting the disease’s progression and may be useful in tackling other neurodegenerative diseases caused by protein aggregation.
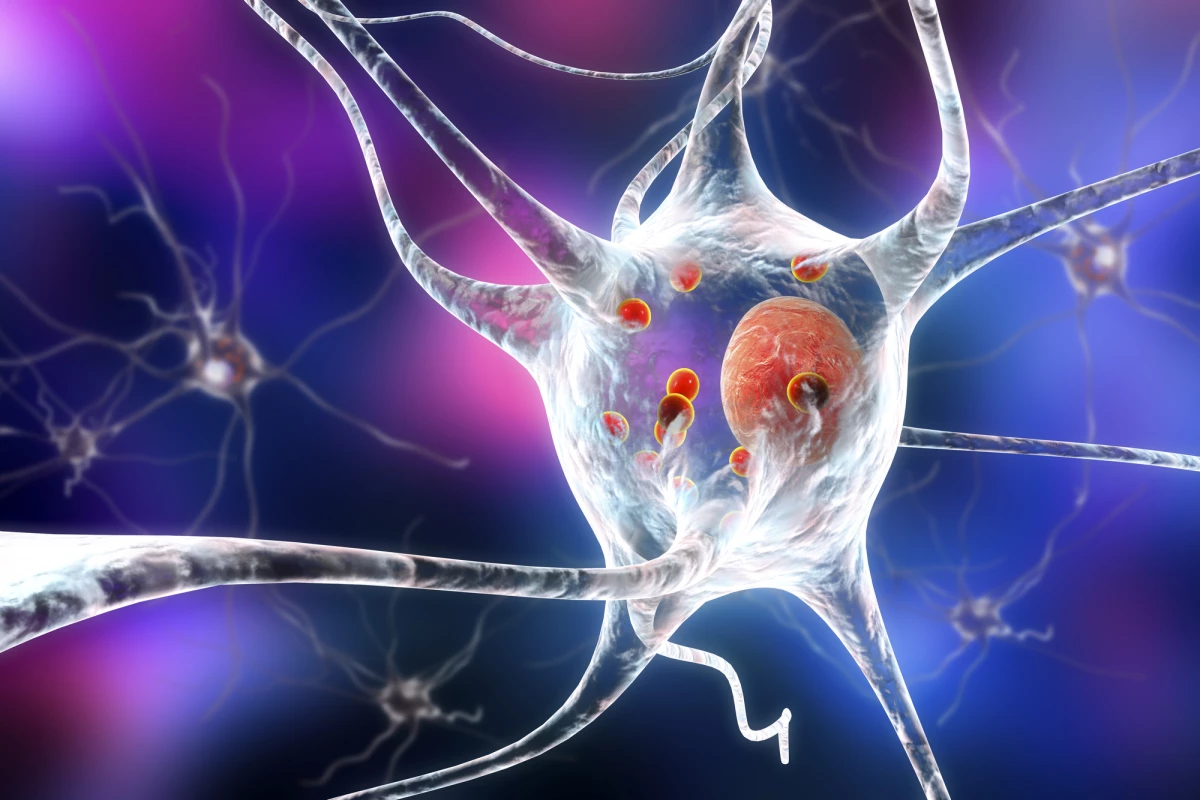
More than 20 years ago, the protein alpha-synuclein was discovered to have a critical role in the development of Parkinson’s disease (PD). Toxic, mutated alpha-synuclein are thought to clump together to form Lewy bodies, leading to progressive neuronal death. Alpha-synuclein has also been implicated in the second most common form of dementia after Alzheimer’s disease, Lewy body dementia.
The association between neurodegenerative disorders and the aggregation and spread of proteins such as alpha-synuclein has been well-researched. But what remains unclear is what comes first: aggregation or spread. A new study by researchers at the Tokyo Medical and Dental University has provided answers.
“Most experiments conducted so far only used fibrils, which are the clumps formed when monomeric alpha-synuclein aggregates,” said Kyota Fujita, the study’s lead author. “The fibrils are transmitted from neurons to neurons, but it remains unclear whether monomers act in the same way.”
To see how monomers and fibrils of alpha-synuclein moved around the brain, the researchers injected a small amount of mutated alpha-synuclein with a green fluorescent protein into the brains of mice. Because any cell can contribute to the spread of alpha-synuclein, they used viral particles to enable its synthesis in the cells at the injection site.
Two weeks after injection, the researchers noticed fluorescence in remote brain regions away from the injection site, indicating the monomeric mutated alpha-synuclein was spreading. They found the fluorescent protein in the glymphatic system, a unique arrangement of channels that eliminates proteins and metabolites from the central nervous system, and noticed that it had been taken up by neurons. When they checked 12 months later, the monomers had clumped together to form fibrils.
“Fibrils of alpha-synuclein formed after the monomers had propagated,” said Hitoshi Okazawa, corresponding author of the study. “Specifically, we observed alpha-synuclein monomer in the glymphatic system and remote regions as early as two weeks after injection, while we found alpha-synuclein fibrils 12 months after injection!”
The researchers noted that the amount of alpha-synuclein aggregation and the time it took to form varied and was not proportional to the distance from the injection site.
They say the study provides an improved understanding of how the alpha-synuclein travels through the brain and may be used to target its spread early in PD development, limiting the disease’s progression. And, they say, the findings could be generalized to other proteins that cause neurodegenerative diseases.
The study was published in the journal Cell Reports.