Noise-induced hearing loss (NIHL) can occur from a one-off exposure to an intense burst of sound, like a gunshot or explosion, or continuous exposure to loud sounds over an extended period, such as in a noisy work environment. With society's increasing industrialization and urbanization, NIHL has become a prevalent problem that affects people of all ages.
Current treatments include hearing aids and cochlear implants, but their effectiveness depends on the number and functionality of surviving sound-detecting hair cells in the inner ear. They can’t reverse the damage done. However, a group of Chinese researchers has developed a novel treatment that combines the principles of traditional medicine and our modern understanding of the gut microbiome to prevent and repair hearing loss.
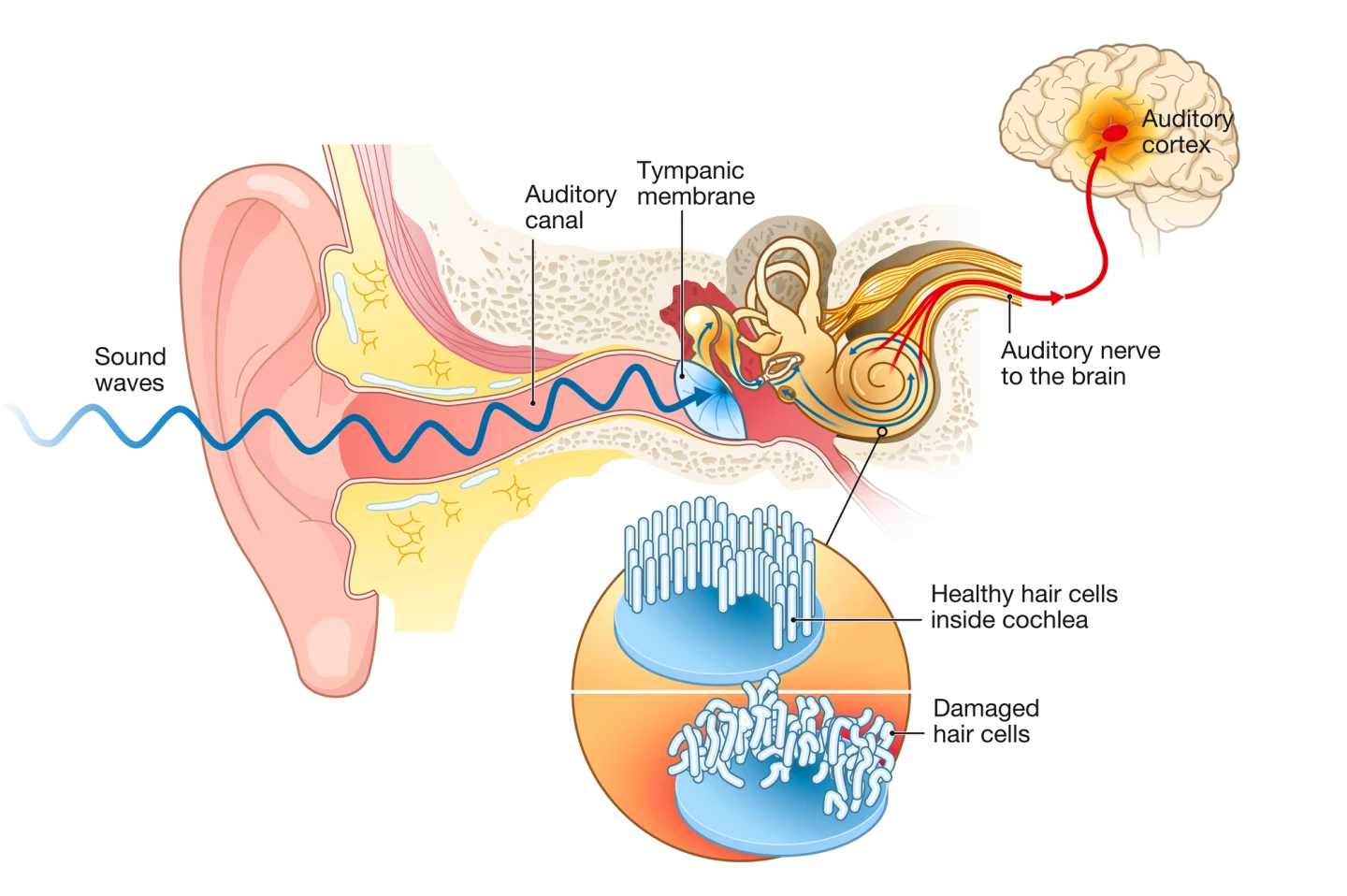
In healthy ears, sound waves travel to the inner ear and into the snail-shaped cochlea. Hair cells in the cochlea pick up the sound waves and start moving up and down, causing microscopic projections on top of the cells to bump against an overlying structure and bend. Bending causes channels to open, causing chemicals to rush into the cells and creating electrical signals that travel along the auditory nerve to the brain, where they’re registered as sound.
With most NIHL, overexposure to noise causes inflammation and the accumulation of damaging reactive oxygen species (ROS) in the hair cells, eventually resulting in their death.
For centuries, magnetite and hematite have been used in traditional Chinese medicine to treat neurological conditions, including hearing loss. Magnetite is believed to possess anti-inflammatory properties and improve blood circulation, among other health benefits. Hematite is said to promote circulation and physical and emotional well-being. Both are magnetic, a property the researchers recreated in their treatment.
They developed a superparamagnetic iron oxide nanoparticle assembly (SPIOCA); essentially a structured collection of nanoparticles of iron oxide, which has magnetic properties. SPIOCA was coated with FDA-approved carboxymethyl cellulose (CMC), a water-soluble cellulose derivative, to ensure it could be taken orally. SPIOCA was also responsive to pH, meaning it could survive the harsh, acidic conditions of the stomach without breaking down.
The researchers tested the effectiveness of SPIOCA against NIHL in mice, giving them the oral iron treatment and then exposing them to white noise (110 dB) for two hours. Pre-treating the mice with SPIOCA before noise exposure promoted hair cell survival.
They also found that SPIOCA was mainly distributed in the gut. Looking closer, they observed that while noise exposure significantly negatively altered the composition of the gut microbiome, SPIOCA corrected it. The increase in ‘bad’ bacteria caused by noise exposure, which are associated with inflammation and infection, was reduced “remarkably” by the treatment.
“Collectively, these results suggested that the benefits of SPIOCA can be attributed to the modulation of the gut microbiome,” said the researchers.
Previous research demonstrated the link between the gut and the brain and how circulating pro-inflammatory factors resulting from an unbalanced microbiome disrupt the protective blood-brain barrier (BBB) and can lead to brain inflammation. The blood-labyrinth barrier (BLB) in the inner ear protects the cochlea from inflammatory factors in a similar way. The researchers found that SPIOCA inhibited those gut-related inflammatory factors and, by extension, protected against damage caused by resulting cochlear inflammation.
One of the species of beneficial gut bacteria that SPIOCA increased was Bacteroides. These bacteria produce a class of lipids called sphingolipids, which play a crucial role in cell structure and functioning. The researchers found that noise exposure suppressed the expression of a particular sphingolipid receptor in cochlear hair cells, S1PR2, which protects against hearing loss. SPIOCA treatment, however, reversed that inhibited expression.
“This study demonstrates a novel mechanism whereby the gut microbiota influences cochlear inflammation, providing valuable insights into the field of hearing protection,” the researchers concluded. “Additionally, it reveals, for the first time, the positive restorative effect of iron oxide nanomaterials on dysbiotic gut microbiota. By targeting the modulation of gut microbiota, SPIOCA has the potential to become an effective nanomedicine for the treatment of NIHL.”
Further research is needed to understand the mechanisms by which SPIOCA exerts its effects on the gut microbiome.
The study was published in the journal National Science Review.







