Using a cold plasma jet to activate hydrogel, researchers have created a dressing with antibacterial and wound-healing properties. The technology could be used as an alternative to current treatments that rely on antibiotics to treat chronic wounds, such as diabetic foot ulcers.
The growing global number of diabetics means that there will be more people who experience a foot ulcer in their lifetime. For 60% of diabetics, these ulcers will become infected, and because of poor wound healing associated with the condition, the ulcers often become chronic wounds.
Chronic-wound management is aimed at controlling infection and stimulating healing, but it’s limited. Currently, dressings impregnated with antimicrobial silver or antibiotics are the benchmark, which can become less effective due to antibiotic resistance and the potential for silver toxicity. Researchers from the University of South Australia (Uni SA) have investigated a new technology to control infection and stimulate healing: a hydrogel activated by cold plasma ionized gas.
“Antibiotics and silver dressing are commonly used to treat chronic wounds, but both have drawbacks,” said Endre Szili, a corresponding author of the study. “Growing resistance to antibiotics is a global challenge, and there are also major concerns over silver-induced toxicity. In Europe, silver dressings are being phased out for this reason.”
Previous studies have demonstrated the benefits of using cold plasma ionized gas for wound healing, namely reducing bacterial load and generating reactive oxygen and nitrogen species (RONS) by activating the oxygen and nitrogen molecules in the ambient air. Until now, a hydrogel has been loaded with plasma-generated RONS before being applied to a wound, but the procedure isn’t perfect.
“Despite recent encouraging results in the use of plasma-activated hydrogel therapy (PAHT), we faced the challenge of loading hydrogels with sufficient concentrations of RONS required for clinical use,” Szili said. “We have overcome this hurdle by employing a new electrochemical method that enhances the hydrogel activation.”
The researchers created their hydrogel using poly(vinyl alcohol) (PVA) because of its widespread regulatory approval for healthcare use and excellent mechanical and biocompatible properties. The PVA hydrogel was treated with a helium plasma jet to activate it, generating RONS. An 8% PVA hydrogel was determined to be optimal as a PAHT dressing because it could be readily activated by plasma-generating RONS while retaining its structural integrity, conformability, and ability to swell.
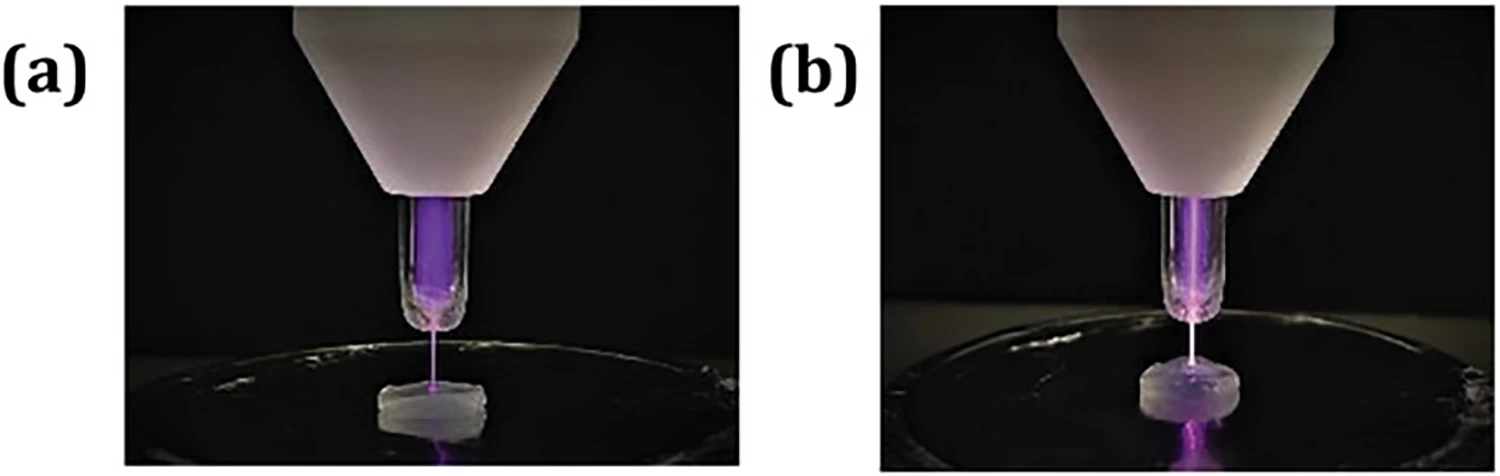
Positioning the hydrogel above an aluminum plate so the plasma plume remained in contact with it during treatment, the researchers compared two techniques to see whether RONS production could be electrochemically enhanced: either the hydrogel was kept at ‘floating potential’ by disconnecting the aluminum plate from a grounded wire, or it was ‘grounded’.

Plasma-treated hydrogels were incubated for three hours to study the release of hydrogen peroxide (H2O2) and nitrous oxide (NO2-), which were used as markers for total reactive oxygen species (ROS) and reactive nitrogen species (RNS), respectively. The researchers found that grounding the hydrogel during plasma treatment significantly enhanced H2O2 production and that H2O2 production was further enhanced by hydrating the gel during treatment. Additionally, humidity at the plasma jet-hydrogel interface was closely correlated with increased H2O2 production. Regarding NO2-, grounding increased production by humidity and hydration had a negligible effect.
During in vitro experiments, the hydrogel was highly effective at controlling the growth of E. coli and P. aeruginosa, two bacteria commonly found in diabetic foot ulcers. Although the study focused on diabetic wounds, the researchers say that the technology could be used to treat all chronic wounds and internal infections.
“A major advantage of our PAHT technology is that it can be used for treating all wounds,” Szili said. “It is an environmentally safe treatment that uses the natural components in air and water to make its active ingredients, which degrade to non-toxic and biocompatible components.”
The next step is to move to clinical trials to optimize the electrochemical technology for treating human patients. The researchers will, in future, look at using the tech to treat cancerous tumors by activating drugs contained within hydrogels injected into the body.
“The active ingredients could be delivered over a lengthy period, improving treatment, with a better chance of penetrating a tumor,” said Szili. “Plasma has massive potential in the medical world, and this is just the tip of the iceberg.”
The study was published in the journal Advanced Functional Materials.
This video explains how the plasma-treated hydrogel works.
Source: Uni SA