Injections of pain-relief medication into the affected joints is one of the primary ways physicians treat discomfort in sufferers of osteoarthritis, but the effects don’t last forever. A novel technique that involves directing low-grade radiofrequency energy through sensory nerves to block pain is shaping as a promising alternative, after delivering significant and long-lasting decreases in pain in an early study.
Opioid-based painkillers are one option for sufferers of osteoarthritis, which affects the flexible tissues at the ends of the bones, but these bring the risk of addiction. Injections of other pain-relievers like anesthetics and corticosteroids offer an alternative, but as Dr Felix M. Gonzalez from the Emory University School of Medicine explains, these too have their limitations.
“Usually, over time patients become less responsive to these injections,” he says. “The first anesthetic-corticosteroid injection may provide six months of pain relief, the second may last three months, and the third may last only a month. Gradually, the degree of pain relief becomes nonsignificant.”
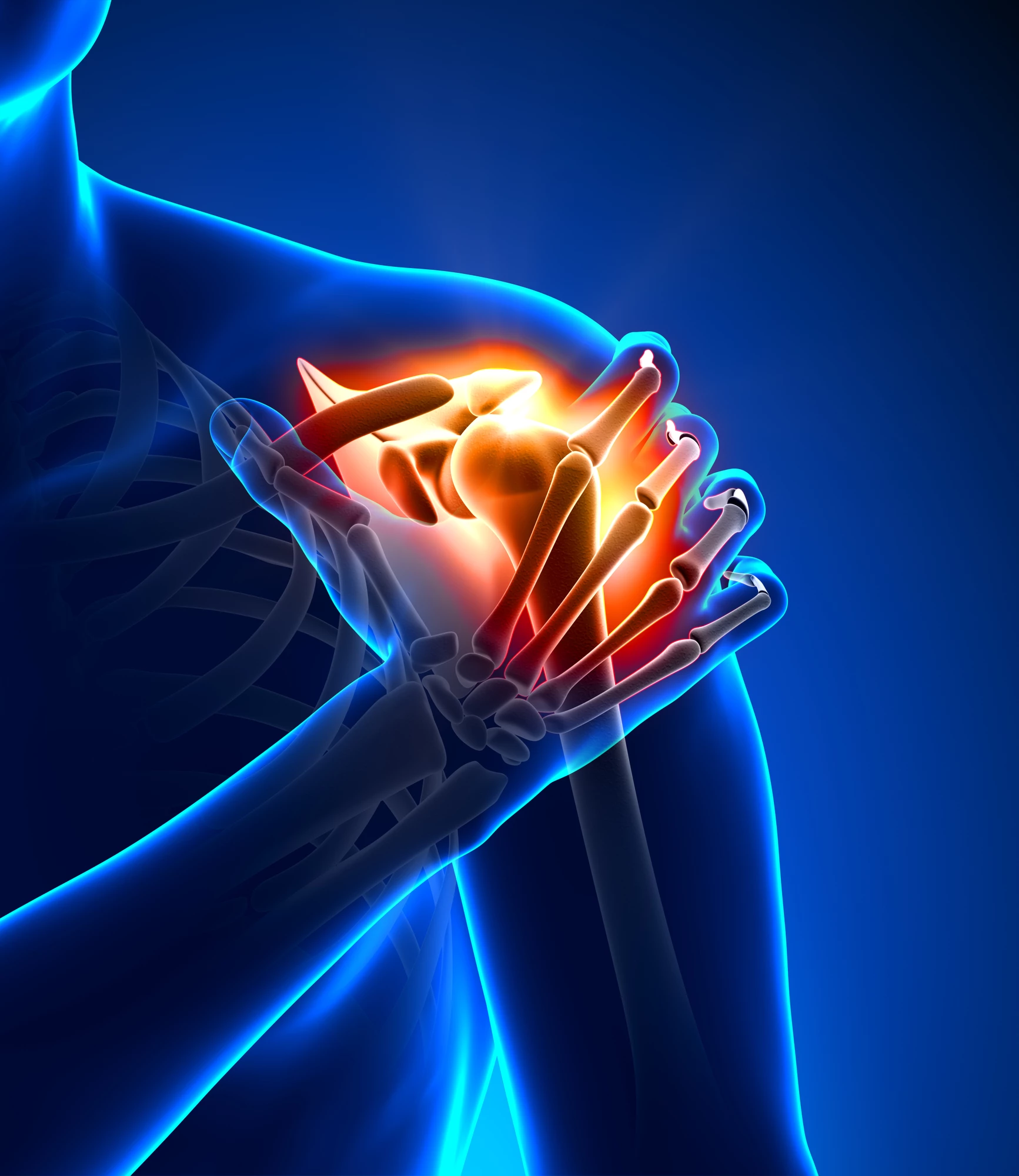
Gonzalez and his team see another possibility in what’s known as cooled radiofrequency ablation. This emerging form of targeted pain relief involves inserting needles into the affected joint to deliver low-grade radiofrequency energy that “stuns” the sensory nerves.
This has the effect of slowing the transmission of pain signals to the brain, and last year Gonzalez and his team carried out a study where they used a similar technique to successfully treat pain in knee arthritis patients. The scientists have now turned their attention to shoulder and hip arthritis, enlisting 23 patients that had become unresponsive to anti-inflammatory pain control and steroid injections.
The subjects received the cooled radiofrequency ablation treatment and then completed surveys relating to their pain, range of motion and joint function three months after the procedures. Both hip and shoulder pain groups reported significant decreases in pain and increases in dynamic function as a result of the therapy.
“In our study, the results were very impressive and promising,” Dr. Gonzalez says. “The patients with shoulder pain had a decrease in pain of 85 percent, and an increase in function of approximately 74 percent. In patients with hip pain, there was a 70 percent reduction in pain, and a gain in function of approximately 66 percent.”
The scientists see this therapy potentially filling a hole in treatment options for arthritis patients who aren’t responding to injections of pain-relieving medications and wish to avoid opioids or full joint replacement surgery. They also believe it may come to treat discomfort driven by other diseases like cancer and sickle cell anemia-related pain syndrome.
“We’re just scratching the surface here,” Dr. Gonzalez says. “We would like to explore efficacy of the treatment on patients in other settings like trauma, amputations and especially in cancer patients with metastatic disease.”
The research is to be presented at the annual meeting of the Radiological Society of North America this month, while a study abstract can be accessed online here.