Directly applying red-light therapy to a damaged spinal cord protects and regenerates nerve cells, leading to a return of motor and sensory function, according to new research. The treatment could expand the currently limited treatments available to people with spinal cord injuries.
Spinal cord injuries (SCIs) caused by things like falls, sporting accidents and road traffic collisions can lead to profound, lifelong disability. Unfortunately, many don’t recover completely, especially if the injury is severe.
The options to repair SCIs remain limited, so researchers have long focused on developing alternative treatments. In a new study, researchers from the University of Birmingham in the UK determined the optimal dose of red-light therapy needed to restore function and stimulate nerve cell growth in an injured spinal cord.
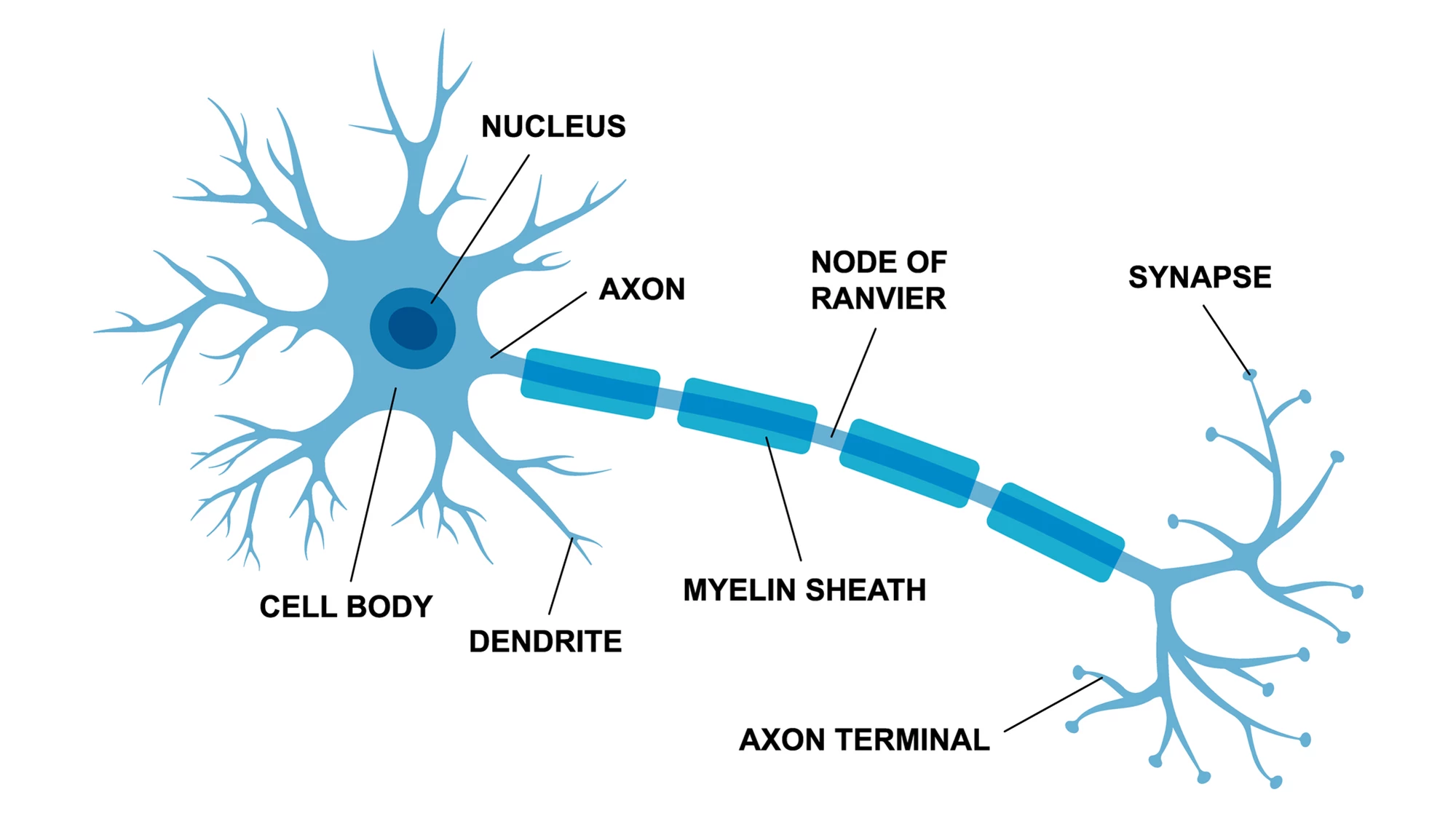
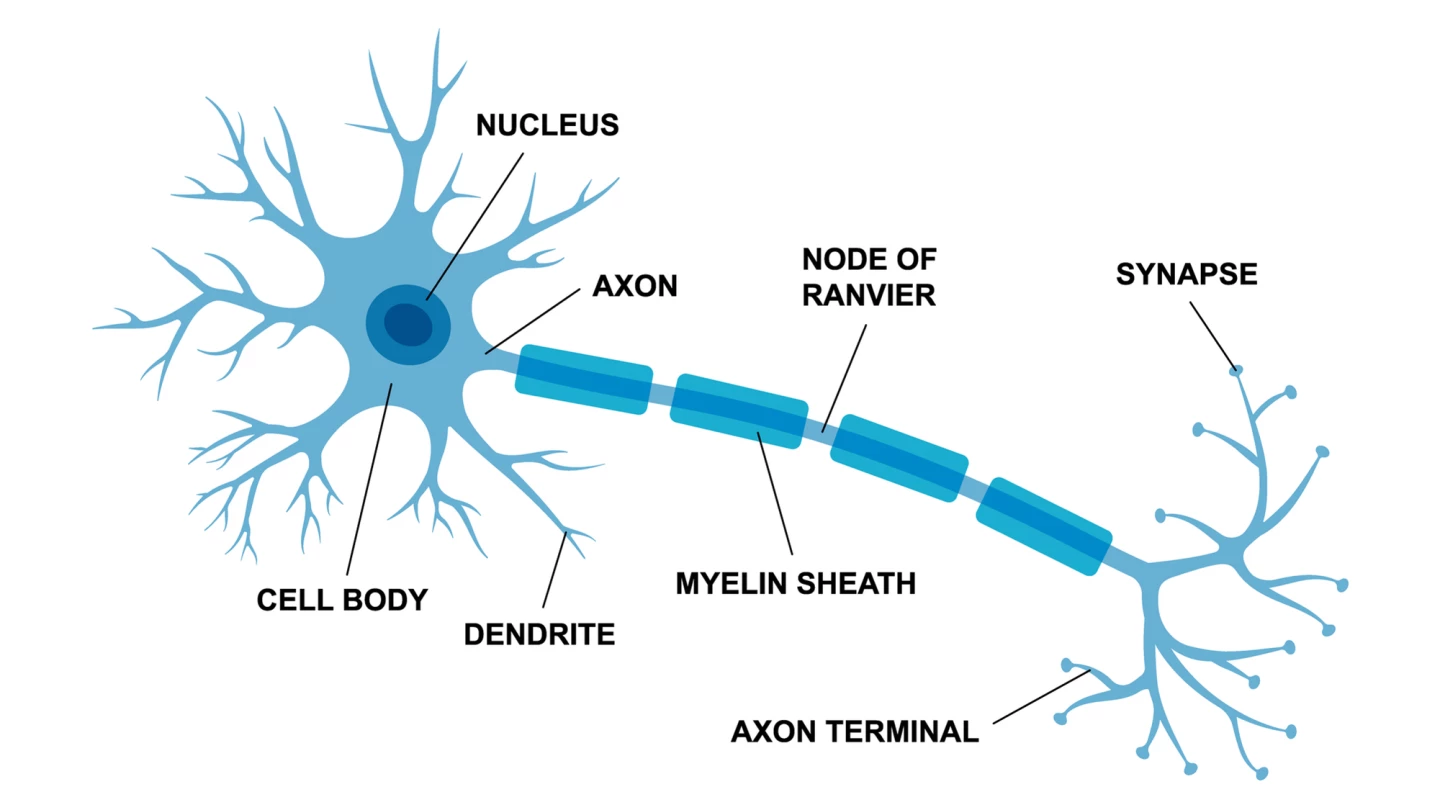
Light therapy, also called photobiomodulation or PBM, involves the application of low-intensity red and near-infrared light from lasers or LEDs to stimulate healing, relieve pain, and reduce inflammation. It may sound a little ‘woo-woo,’ but studies have shown that PBM works at the level of the mitochondria, the cell components responsible for generating energy. It triggers pathways that mitigate brain cell death (apoptosis), nerve cell (neuronal) damage, and neuroinflammation while promoting nerve regeneration. The question the researchers sought to answer was: What dosage of light is needed to elicit a therapeutic effect?
They first created cultures of adult rat nerve cells (neurons) and treated them with PBM, one-minute daily doses delivered by LED at a wavelength of 660 nanometers (nm). Red light sits at the ‘long end’ of the visible light spectrum, with wavelengths of 600 nm to 700 nm (compared with violet, which sits at the lower limit of 400 nm). At 660 nm, red light has been found to penetrate the skin into underlying tissues.
These in vitro experiments showed that, at five days, the number of live cells had increased by 45% with PBM, compared to a control. Treatment also produced an observable increase in the length of neurite outgrowths – small extensions that grow out of neurons to create connections with other neurons.
“Excitingly, this aspect of the study showed the effect of 660 nm light was both neuroprotective, meaning it improved survival of nerve cells, and neuroregenerative, meaning it stimulated nerve cell growth,” said Zubair Ahmed, a professor of neuroscience at the University of Birmingham and the study’s co-corresponding author.
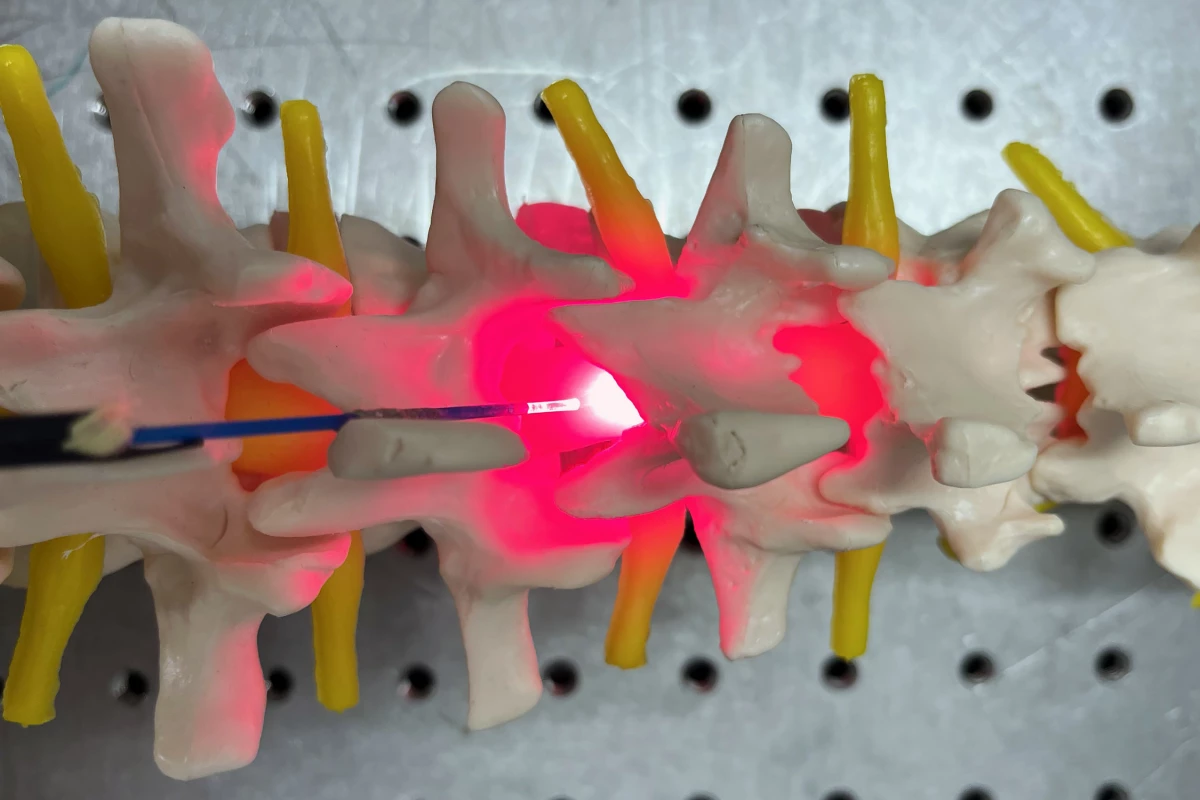
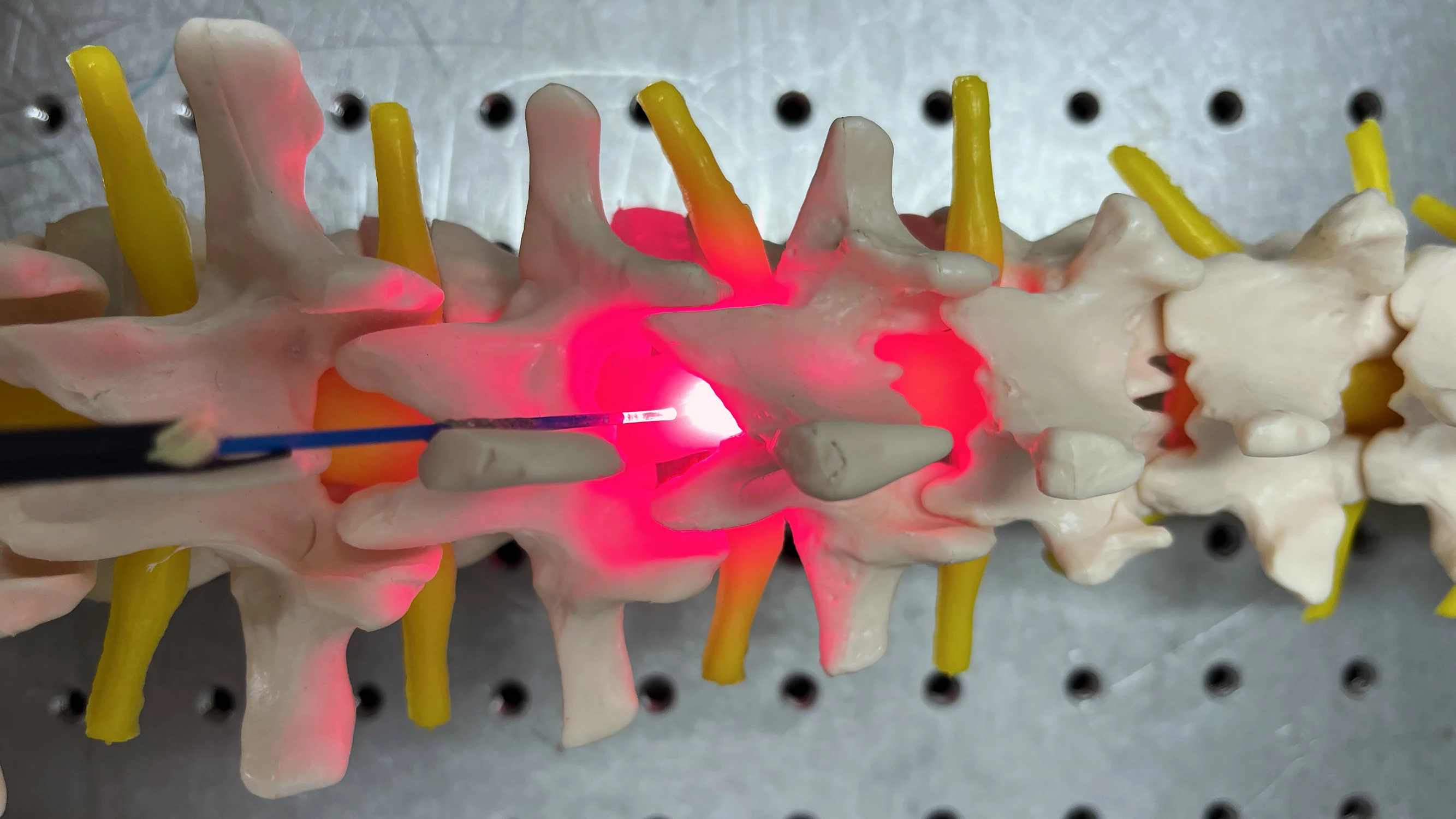
The researchers then undertook in vivo experiments, comparing invasive and noninvasive delivery of PBM to rats with crushed spinal cords. For the invasive arm of the study, a fiber optic catheter was implanted internally to provide PBM directly to the spinal cord. For the noninvasive (transcutaneous or ‘through the skin’) arm, the catheter was placed in direct contact with the skin over the injury site. The first one-minute 660 nm treatment was given 15 minutes post-injury and then repeated daily for seven days.
They found that invasive and noninvasive methods delivered equivalent PBM doses to the SCI site. Both methods increased activation of a regeneration-associated protein at three days post-injury. Axons, the long cables of neurons that carry electrical impulses to other neurons, increased from 18% (control) to 41.4% (invasive method) and 45.8% (noninvasive method). This axonal regeneration led to significant improvements in the rats’ functional motor and sensory recovery at six weeks post-injury and reduced lesion size.
“Surgery after spinal cord injury is common, but currently, these operations are only aimed at stabilizing injuries to the bones of the spine that have been damaged by the trauma,” said Andrew Stevens, neurosurgical registrar and the study’s lead author. “This [light therapy] concept is incredibly exciting as it could offer surgeons the opportunity, during the same operation, to implant a device which could help protect and repair the spinal cord itself.”
This is the first time invasive and noninvasive delivery of PBM has been compared in SCI. The researchers have already received further funding and are planning to develop an implantable device for humans with traumatic spinal injury, where there are no current therapies that preserve neurons or improve neurological function. The researchers are well aware that, anatomically, rats are very different from humans.
“To make light therapy viable for treating SCI in humans, an implantable device will be required to provide line of sight to damaged tissue and the opportunity for greater accuracy and standardized dosing without impedance due to the thickness of skin and other tissues surrounding the spinal cord,” Ahmed said.
The study was published in the journal Bioengineering & Translational Medicine.
Source: University of Birmingham