An osteochondral defect (OCD) is an area of focal damage involving the articular cartilage that lines the joint’s bony surface and a piece of underlying bone. OCDs in the knee can result from arthritis or an acute traumatic injury – a football tackle, for example – that causes arthritis, leading to chronic pain and loss of joint function.
Knee OCDs can be treated conservatively with joint immobilization and pain medications, but if the condition is advanced or severe, surgery is required, including total knee replacement. Now, researchers at Texas A&M University have received a grant from the National Institute of Arthritis and Musculoskeletal and Skin Disease, part of the National Institutes of Health (NIH), to develop their cartilage-capped regenerative osteochondral plugs (CC-ROPs), an off-the-shelf synthetic device that could be an alternative to total knee replacement.
“Chronic knee pain and disability are caused by cartilage loss and OCDs stemming from arthritis, including osteoarthritis and post-traumatic arthritis, causing individuals pain that limits comfort and mobility,” said Melissa Grunlan, a professor in the University’s Department of Biomedical Engineering. “This grant will allow us to maximize the potential of the CC-ROPs to heal OCDs and to collect data demonstrating this efficacy.”
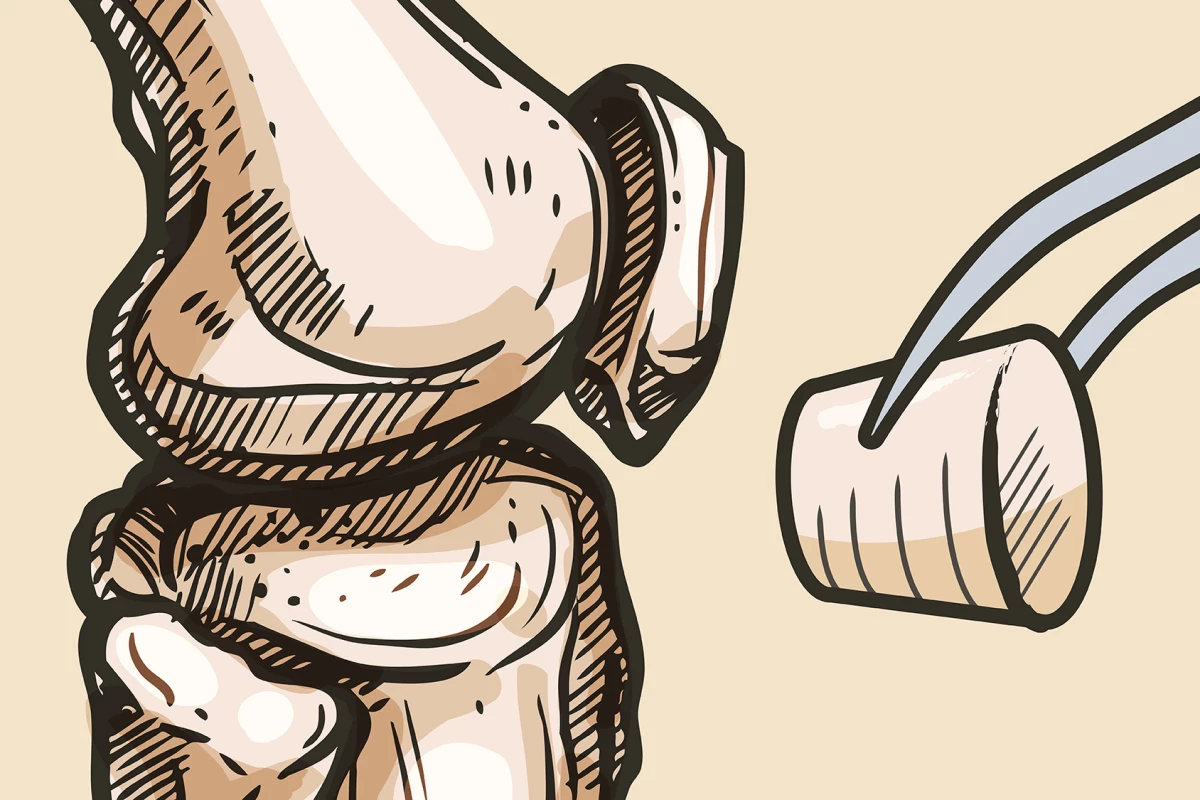
Autografting is commonly the step before total knee replacement surgery. It involves harvesting cylindrical ‘plugs’ from non-damaged sections of the patient’s knee and implanting them in a hole or holes drilled in the affected area. Over time, the implants enable bone and cartilage to grow into the damaged area. However, the procedure’s effectiveness is limited when the patient is older than 40, or the OCD is large. Where autografting is deemed inappropriate, a total knee replacement is sometimes the patient’s only option.

Total knee replacement is extensive surgery, although the name is kind of a misnomer. Only the surfaces of the bones are replaced. The surgeon removes the damaged cartilage and a small amount of underlying bone and replaces it with metal components to recreate the joint surface. A plastic spacer is placed between the metal components to provide a smooth, gliding surface. About 790,000 total knee replacements are done in the US each year.
CC-ROPs comprise an ultra-strong hydrogel cap that mimics the properties of natural cartilage and a porous polymer scaffold base. Because they’re similar to the cylindrical plugs used in autografts, the same protocols and tools can be used. Like autografts, following implantation into a pre-drilled hole, the porous base of the CC-ROP enables the growth of new bone tissue, while the cap provides the ‘cartilage’ needed for joint function. However, unlike autografting, CC-ROPs are not limited by patient age or defect size. And they don’t require pre-loading with cells or growth factors to accelerate healing.
Having now secured funding, the researchers at Texas A&M University can work on maximizing the functionality of CC-ROPs to ensure they’re ready for real-life applications. Planned pre-clinical studies will evaluate the device’s effectiveness.
Source: Texas A&M University