Chronic stress can rewire the brain, leading to a host of mental health issues. Now, scientists believe that one small sugar-adding process may act as a switch for depression, providing new insights into mood disorders – and a new target to treat them.
Scientists from South Korea's Institute for Basic Science (IBS) found that prolonged stress changes how proteins in the medial prefrontal cortex (mPFC) are “decorated” with sialic acid – a sugar molecule that helps shape the surface properties of neurons. These sugar chains, called glycans, are attached after proteins are made, forming the process known as glycosylation. Glycosylation has been studied in terms of how it impacts cancer development and, more recently, neurodegeneration.
One type of glycosylation is O-glycosylation, where sugars attach to oxygen atoms on certain amino acids in a protein. This molecular “sugar coating” helps regulate how neurons connect and signal to one another. Until recently, it was largely overlooked in mental-health research, but scientists are now finding that stress can disturb these sugar patterns, potentially rewiring "normal" communication between brain cells.
In this study, the researchers identified that a single enzyme, St3gal1, performs the final “sugar-capping” step in the process, and this small but integral stage influences how long proteins last and how they interact at synapses – and how, if this falters, it appears to influence depression-like behaviors as a result.
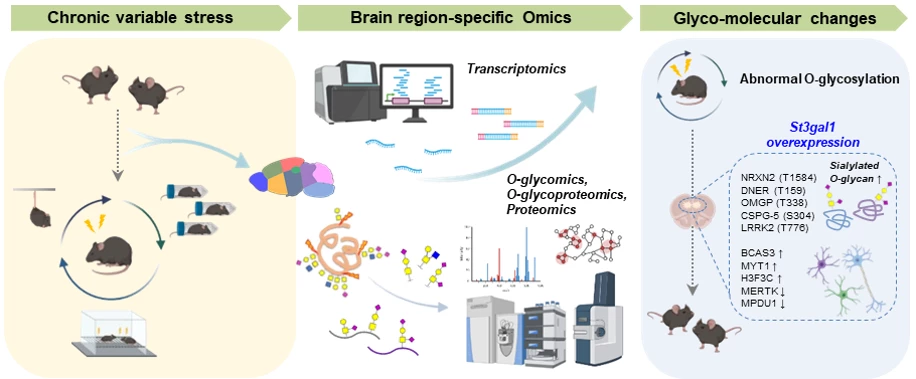
Researchers used high-performance mass spectrometry to map O-glycosylation patterns across nine brain regions in healthy mice. Each area had a distinct sugar signature, reflecting its unique cellular blueprint. When the team compared these with those from chronically stressed mice, they found a significant difference in the prefrontal cortex, a region linked to mood regulation. Here, stress led to a noticeable reduction in that final O-glycosylation sugar-capping step, and a corresponding drop in St3gal1 expression.
Knocking out St3gal1 in healthy mice caused depressive symptoms, including loss of motivation and heightened anxiety. Increasing St3gal1 in stressed mice had the opposite effect, easing those behaviors. This showed that the enzyme has a key role in how stress triggers depression-like changes in the brain. The team also found that St3gal1 helps maintain sugar tags on neurexin-2, a protein that supports communication between neurons. In stressed mice, those tags vanished – along with normal neural signaling – but restoring St3gal1 brought them back.
“This study demonstrates that abnormal glycosylation in the brain is directly connected to the onset of depression,” said research fellow Boyoung Lee. “It provides an important foothold for identifying new diagnostic markers and therapeutic targets beyond neurotransmitters.”
While the findings were only demonstrated in the brains of male mice – and, of course, the neural networks in humans are far more complex – it provides a new angle for research into depression and its treatment. Many current antidepressants act on serotonin – boosting its levels or altering its signaling – but there's growing evidence suggesting that it's not simply a case of "too little serotonin."
“Depression imposes a major social burden, yet current treatments remain limited,” added C. Justin Lee, IBS director. “This achievement could extend not only to depression therapy but also to other mental illnesses such as PTSD and schizophrenia, paving the way for broader therapeutic strategies.”
Interestingly, female mice that experienced chronic stress exhibited behavioral changes but their St3gal1 levels didn't change, suggesting that males and females may rely on different molecular routes to cope with adversity. This too has provided the scientists with another avenue of investigation.
The research was published in the journal Science Advances.
Source: Institute for Basic Science