A new study shows that a personalized, precise form of brain stimulation, HD-tDCS, can rapidly ease depression symptoms – and even reduce anxiety – offering a promising drug-free alternative with only mild side effects.
We’ve reported on research that used transcranial direct current stimulation (tDCS) to improve cognitive functioning and treat depression. tDCS involves delivering a low-intensity direct current via electrodes on the scalp to trigger changes in the excitability of neurons on the brain’s surface or cortex.
In a new study, researchers from UCLA trialed a newer, more precise and more personalized version of tDCS, called high definition tDCS or HD-tDCS, as a way of treating depression.
“By honing in on the precise brain regions affected by depression, we’ve shown that stimulation can significantly improve mood and daily functioning,” said the study’s lead author, Mayank Anant Jog, PhD, assistant professor of neurology at UCLA Health. “Our data indicates that HD-tDCS therapy may also be effective for treating anxiety disorders, though dedicated studies to investigate this possibility are needed.”
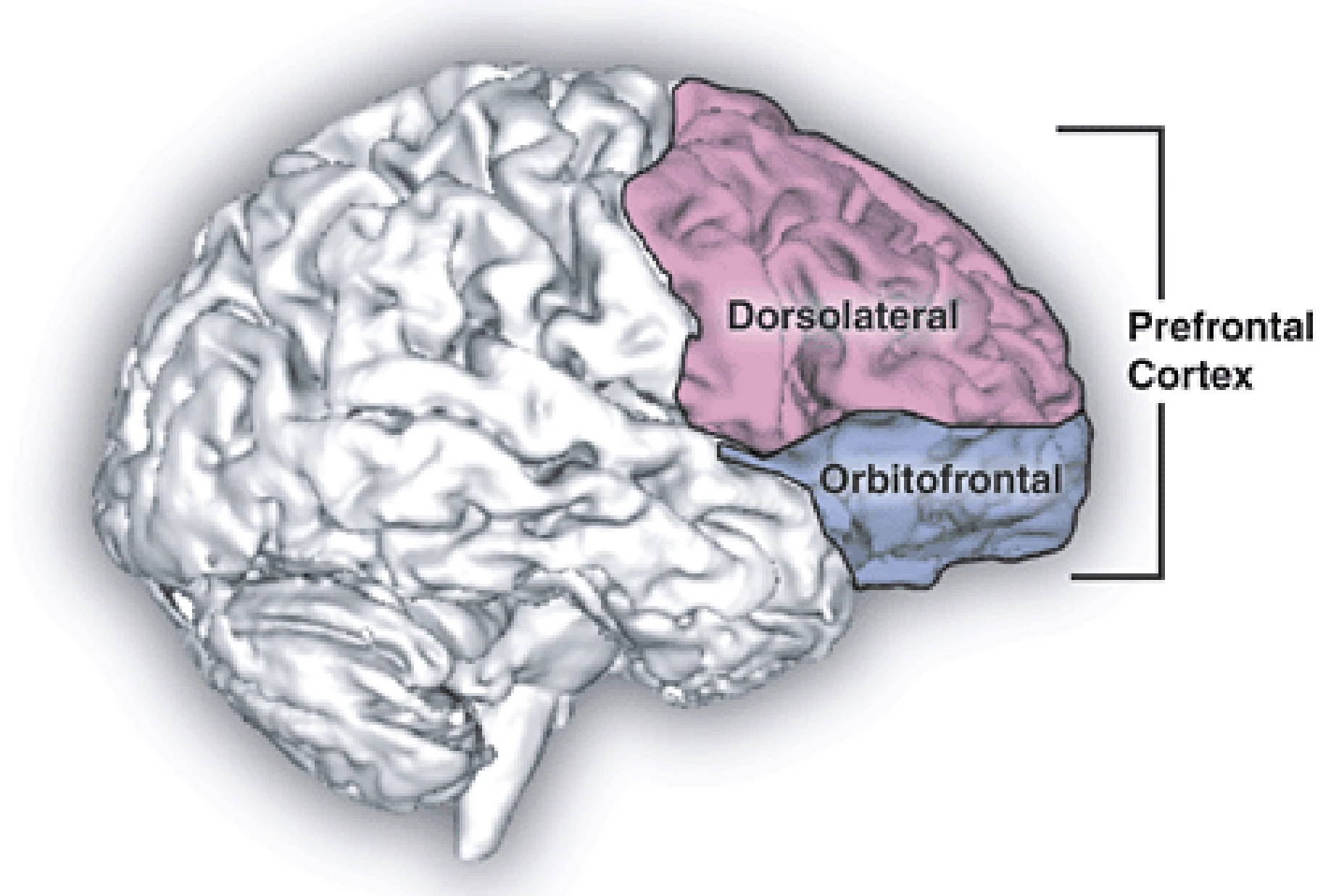
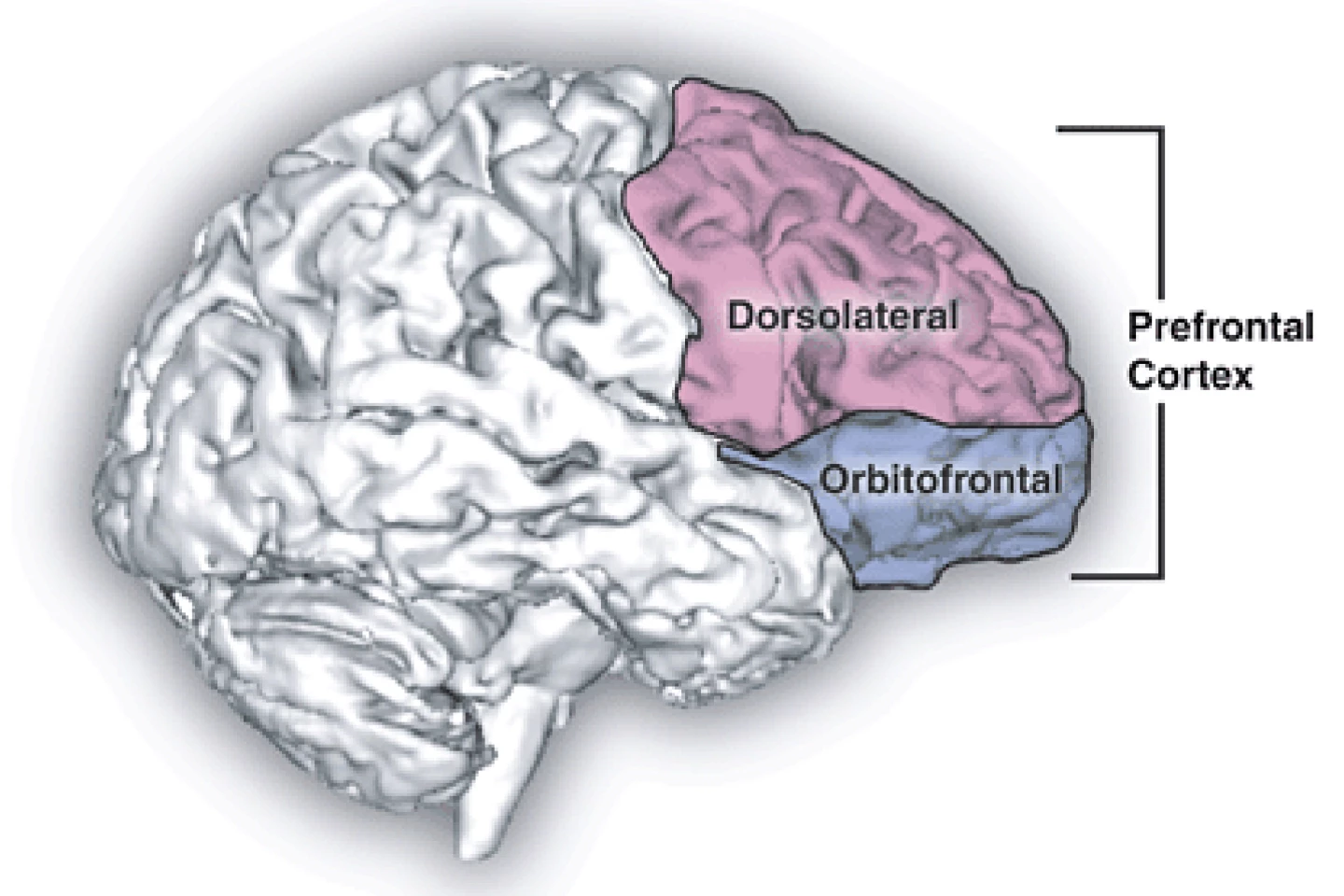
HD-tDCS enables more precise targeting of specific cortical regions by using a combination of smaller electrodes in combination with neuroimaging to determine the optimal brain target. In the present trial, the researchers delivered mild electrical currents to a specific brain area, the left dorsolateral prefrontal cortex (DLPFC), a region often linked to mood regulation.
Sixty-eight adults aged 18 to 65 with moderate to severe – but not treatment-resistant – depression were enrolled in the randomized, double-blind, sham-controlled trial (that is, neither participants nor assessors knew who received real vs. fake treatment). Participants were either taking a stable regimen of antidepressants or not taking them at all. People with bipolar disorder, schizophrenia, or neurological disorders were excluded.
Participants were randomized to receive either active HD-tDCS therapy (at a current of 2 mA) or sham therapy for 20 minutes every day for 12 consecutive working days. This setup was personalized for each participant, using MRI scans and neuronavigation to precisely target the DLPFC. The active group received a current of 2 mA with brief (30-second) periods of ramping, whereas the sham group got a ramp-up/ramp-down current that felt real but wasn’t therapeutically active. The main outcome the researchers were testing for was a change in depression severity using the Hamilton Depression Rating Scale (HAM-D). Secondary measures included remission and response rates, side effects, and exploratory tests for anxiety symptoms.
Depression scores dropped in both groups, but more so in the active HD-tDCS group. The average improvement in the active group was –7.8 points on HAM-D, and in the sham group, –5.6 points. This difference was statistically significant. Regarding remission rates, 39.5% of active participants went into remission (defined as a HAM-D score of ≤ 7), compared to only 13.3% in the sham group.
Some benefits were seen halfway through treatment (day six), suggesting faster improvement than standard antidepressants or psychotherapy, which usually take weeks to produce an effect. Anxiety scores also improved more in the active group, hinting that HD-tDCS could help both depression and anxiety. The treatment was generally well-tolerated. Mild side effects included skin redness, itching, or burning sensations at the electrode site, but these were minimal. No serious adverse effects were reported.
“Overall, the HD-tDCS therapy was effective and well-tolerated, with only mild to no side-effects observed in the study,” said Katherine Narr, a professor in UCLA’s Department of Neurology and the study’s senior author. "Coupled with tDCS’s potential for convenient at-home use, this approach may offer a new treatment option for those seeking alternatives to medication or talk therapy.”
The sample size was smaller than planned, partly due to COVID-19-related recruitment issues. Further, the trial wasn’t designed to examine how HD-tDCS interacted with antidepressants, so any combined effects remain unclear. While the sham group only received a very tiny current, it may not have been completely inert. Participants were only tracked for four weeks after treatment, so the long-term effectiveness of the treatment isn’t known. It’s unknown whether the effects fade without the administration of “booster” sessions. And, while treatment was individualized, the researchers didn’t directly compare personalized vs. non-personalized HD-tDCS.
Despite these limitations, HD-tDCS could become a fast-acting, non-drug option for people with moderate to severe depression, especially those who can’t tolerate medication side effects. If refined, this kind of treatment could be adapted for safe, at-home treatments in the future. It’s promising that HD-tDCS also lowered anxiety.
Follow-up studies could test whether mood improvements continue during a longer treatment period with appropriate maintenance treatments.
The study was published in the journal JAMA Network Open.
Source: UCLA Health