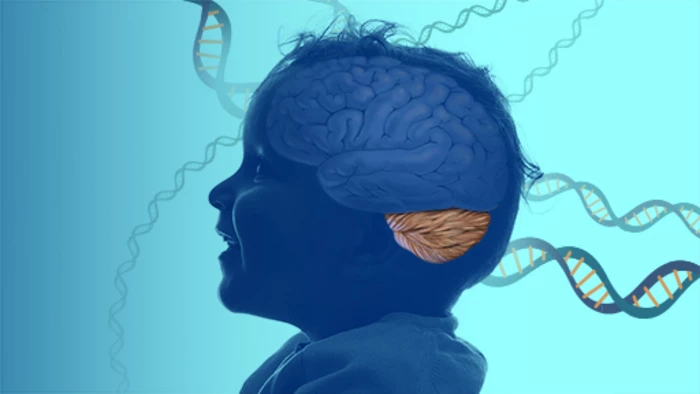
A neurological disorder that causes issues with speech and motor coordination has been identified in three children by scientists from the National Institutes of Health's National Human Genome Research Institute (NHGRI) and Undiagnosed Diseases Program. The researchers believe the condition is caused by a genetic mutation that affects the ability of neurons in the brain to properly carry out a cellular recycling function called autophagy. In addition to helping those afflicted with the condition, the scientists hope the discovery could help evaluate other diseases in which autophagy is implicated, such as Alzheimer's.
The first subject in the study presented with symptoms at age three. He had an abnormal gait, reduced coordination, and would get lost in staring episodes. As the boy aged, he experienced seizures, decreased reflexes and speech patterns that were only 60-75% intelligible. At age nine-and-a-half, the boy was diagnosed with ADHD, mild cognitive impairment, and oppositional defiant disorder, a condition that is marked by irritability and anger, as well as arguing with parents and other authority figures. The boy has a sister who, despite having early development issues, has grown up with no symptoms of the disease.
The other two subjects are both affected sisters. One experienced abnormal hand movements, tripping episodes and periods of staring as a child, and has been left with a mild learning disability and speech difficulties. The other sister also had issues with motor control which eventually resolved, although she has also been left with challenges related to articulating words.
In examining the children's health records, the NIH researchers discovered that they all had mutations in a gene known as ATG4D. Scientists knew from a 2015 study that a mutation in this gene caused issues with motor control and eye movement in Lagotto Romagnolo dogs, but they had yet to link the mutation to issues in human subjects.
To find out if ATG4D mutations were causing the issue in children, the researchers inserted the children's mutations into cells in a lab dish. They discovered that the affected cells couldn't carry out autophagy, a process in which all cells break down old or damaged proteins for reuse when needed. Enhanced autophagy has been linked to fewer clogged arteries and longer lifespans in mice, while research published last year shows that the autophagy process can be manipulated to reduce the amount of plaque-causing proteins that build up in the brain, eventually leading to Alzheimer's disease.
Interestingly, the researchers found that the ATG4D mutation in the skin cells of the affected children didn't interfere with autophagy. It was only in the brain that the mutation altered the cellular recycling system.
"The brain is so complex, and neurons have very specialized functions," said May Christine Malicdan, NHGRI staff scientist and senior author of the study. "To fit those functions, different neurons use different genes, so changes in redundant genes can have major impacts in the brain." Because autophagy is implicated in Alzheimer's and Parkinson's diseases, the researchers hope that their work can lead to breakthroughs in associated research.
"That’s the million-dollar question in rare disease research," said Malicdan. "Rare diseases can help us understand biological pathways, so we can better understand how those pathways contribute to other rare and common conditions."
Going forward, the researchers will continue to work with the three children in the study and seek others afflicted by the disorder.
The study has been published in the journal npj Genomic Medicine.