Researchers have successfully developed nerve grafts, currently being trialed as a treatment for Parkinson’s disease, that are invisible to the body’s immune system, according to a new study. It could mean risky post-transplant anti-rejection drugs are soon a thing of the past.
With ongoing advances in medical technology, cell therapy using stem-cell-derived products is becoming a realistic prospect for treating many diseases. That includes Parkinson’s disease, where preclinical and clinical studies have evaluated the use of nerve, or neural, grafts.
A big problem with introducing grafts into the body is that they’re considered foreign objects, and unless anti-rejection drugs are given, the immune system targets them. Now, research led by The Florey Institute of Neuroscience and Mental Health (The Florey) in Australia has developed an ingenious way of avoiding that problem.
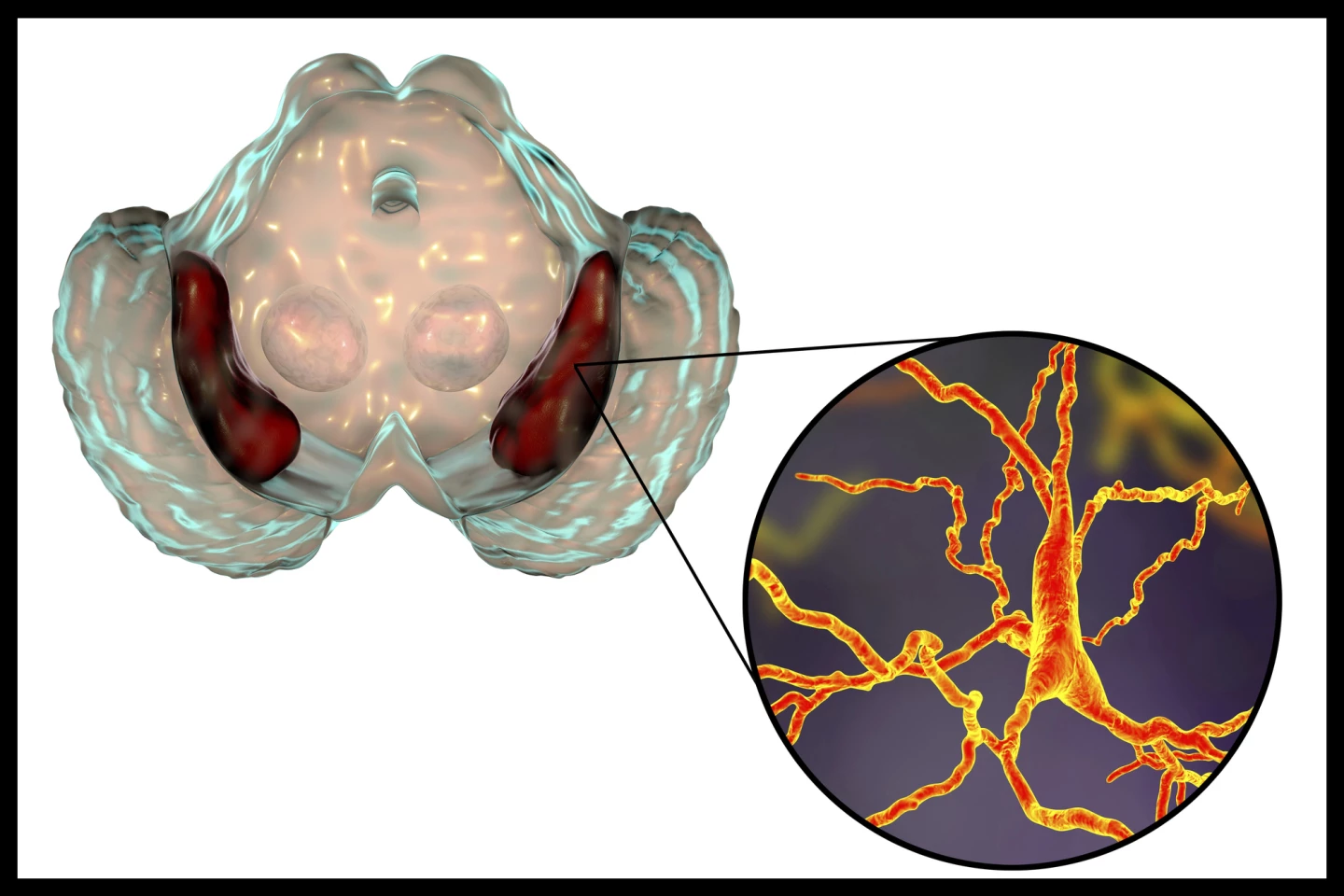
“Parkinson’s disease causes specific nerve cells – neurons – to die, leading to symptoms that include difficulties moving, tremor, stiffness, and impaired balance,” said Florey Deputy Director Professor Clare Parish, Head of the Stem Cells and Neural Development Group and the study’s lead author. “Neural grafting is an emerging treatment to replace those dead neurons.
“Human neural graft trials are underway overseas but, as with other types of organ or cell transplants, patients need to stop their body rejecting the graft by taking immunosuppressant drugs several times a day. Unfortunately, these drugs carry their own risks and side effects.”
In stem-cell-derived neural grafting, human pluripotent stem cells (hPSCs), adult cells such as skin cells reprogrammed to act like stem cells again, are guided to develop into dopamine-producing (dopaminergic) neurons. These are the kinds of neurons that are destroyed in Parkinson’s disease. The dopaminergic neurons are grown in a lab and then transplanted into the brain.
Immunosuppressant, or anti-rejection, drugs help calm the immune system down so it doesn’t destroy the newly transplanted cells. In effect, they turn down the volume of the body’s natural defense system. Although there are different types, these medications generally block immune system signals that would ordinarily activate an attack, slow down or reduce the number of immune cells, and prevent inflammation that could damage the graft.
However, turning down the immune system means it’s less able to fight infections, so even mild illnesses like colds or the flu can become very serious. It can also mean that the body might not detect and fight early cancer cells as effectively. Then there are the side effects: gastrointestinal upset, high blood pressure, tremors, weight gain and mood changes.
For the present study, the researchers engineered hPSCs to “overexpress 8 immunomodulatory transgenes.” What does that mean? Let’s break it down. Overexpression just means making lots of something. "Immunomodulatory' is something that calms or adjusts the immune system. And transgenes are genes scientists have inserted into a cell that weren’t there originally. So, what does this engineering do? It allows the stem-cell-derived neurons that comprise the graft to evade the immune system.
“We’ve engineered neurons which are like those currently in clinical trials for Parkinson’s disease, but we’ve also given them an invisibility cloak,” Parish said. “They can hide in plain sight from the immune system. This could mean an end to the need for anti-rejection drugs.”
The engineered grafts were tested in “humanized” mice whose immune systems have been altered to mimic ours.
“After receiving the neuronal graft, the mice showed no negative effects – which is a good indication that the human immune system will accept the neurons,” said the paper’s co-lead author, Dr Chiara Pavan, a neuroimmunology specialist at The Florey. “In rats, the symptoms of Parkinson’s disease were abolished, indicating the cloaked neurons don’t lose their effectiveness against the disease.”
The neurons have also been fitted with an “off switch,” meaning they can be turned off as needed to reduce the risk of tumors developing from grafts. The researchers say their work has tremendous potential, not just for people with Parkinson’s disease.
“We’ve made a cell product that in future could be implanted in people with Parkinson’s disease, reducing the need for anti-rejection drugs,” said Parish. “Stem cells can be turned into any kind of cell, and we’ve effectively made them invisible to the immune system. This is the next generation of neurological treatment, and it could be used as a safe, off-the-shelf product suitable for treating diseases for which cell-based therapies are a viable option, such as stroke, Huntington’s disease, heart disease and diabetes.”
Also involved in the research were the University of Melbourne, Monash University, The University of Sydney, the Walter and Eliza Hall Institute (WEHI), and the Centenary Institute of Cancer Medicine and Cell Biology in Australia, and the Mount Sinai Hospital in Toronto, Canada,
The study was published in the journal Cell Stem Cell.
Source: The Florey






