A new study has confirmed that weight loss or bariatric surgery is safe and very effective, and, for a large percentage of people who were diabetic before the surgery, meant that they didn’t require diabetes medication five years after.
We’ve seen a steep rise in the popularity of injectable anti-obesity drugs like semaglutide as a means of dropping pounds quickly. But they aren’t right for everyone. Some people can’t or won’t use them because of their cost, side effects, and the risk that the weight will return when the drugs are stopped.
Now, new research from Monash University has reminded everyone that before there were injectable weight loss drugs, there was bariatric surgery. The recently published study confirmed that the surgery was safe, produced substantial weight loss, and even got many diabetic patients off their medications.
“This is the first time that it has been shown that the positive effects of bariatric surgery can be delivered in the general community, not just at expert centers, and the first time that the results have been shown to be durable at five years at a community level,” said the study’s lead and corresponding author, Professor Wendy Brown, Chair of Monash University’s Department of Surgery.

According to its website, the Bariatric Surgery Registry (BSR) is “predominantly a quality and safety registry” that monitors and evaluates outcomes for patients who have undergone bariatric surgery in private and public hospitals across Australia and New Zealand. For the present study, BSR data was collected from 122,567 patients who underwent 134,625 completed bariatric procedures in Australia between February 2012 and December 2021.
You’ll notice that the number of completed procedures is larger than the number of patients. That’s because the BSR collects information about primary bariatric procedures, the first time a patient has a procedure, and revisional bariatric procedures. Revisional procedures are performed subsequent to primary procedures and are grouped as corrective (done to correct an issue), reversals (removing a gastric band, undoing the effect of gastric bypass), or conversions (one type of bariatric surgery is changed to another). For clarity, the present study included 102,297 primary procedures and 32,328 revisional procedures. The majority (79%) of participants were female. The average age on the day of any bariatric surgery was 44.
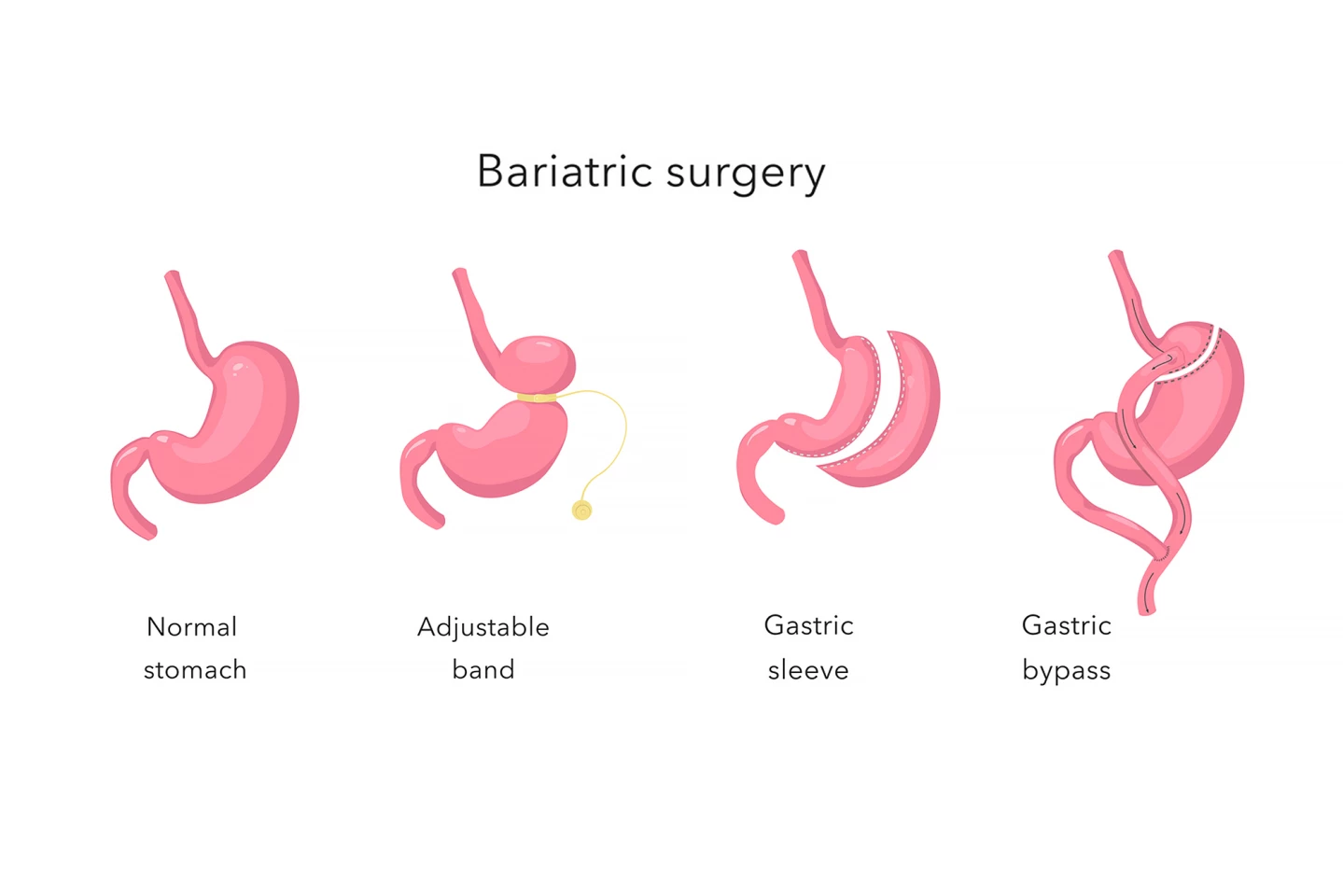
The study looked at data on four different bariatric surgical procedures, each of which are done laparoscopically:
- One-anastomosis gastric bypass (OAGB). A pouch about the size and shape of a small banana is created from the upper part of the stomach. A loop of the small intestine is pulled up and attached to the smaller stomach, meaning that food skips part of the digestive tract, leading to fewer calories and nutrients being absorbed. The larger remaining stomach remains in the body, producing digestive juices that aid digestion. OAGB only requires one connection (anastomosis) between the stomach and intestine, unlike the traditional approach, Roux-en-Y, which requires two.
- Roux-en-Y gastric bypass (RYGB). A small pouch, about the size of an egg, is created from the upper part of the stomach. The small intestine is separated into two sections. The lower portion is connected directly to the new stomach pouch, allowing food to pass directly into the small intestine, where digestion continues but fewer calories and nutrients are absorbed. The upper portion of the small intestine is reconnected to the lower portion, so digestive enzymes from the remaining stomach meet up with the food at the connection point, digesting it.
- Sleeve gastrectomy. About 70% to 80% of the stomach is permanently removed, leaving a tube-shaped stomach about the size and shape of a banana. Food still travels through the normal digestive pathway.
- Adjustable gastric bands. An adjustable band is placed around the top part of the stomach to create a small pouch.
At five years, the total body weight loss for participants who’d undergone OAGB was 34.88%; for those who’d had RYGB, it was 30.73%; for sleeve gastrectomy, 26.5%; and for gastric banding, 17.6%. Along with significant weight loss, the researchers saw a major change in diabetes treatment. Before surgery, 13,904 or 13.6% of participants were recorded as being treated for diabetes. Of this cohort, 57.8% were followed up at 12 months and 71.6% of them reported no longer requiring diabetes medication. For the 22% who were followed up after five years, 61% were no longer taking meds for the condition.
The BSR recorded 148 participant deaths: 0.1%. Of those, 29 were assessed as possibly or definitely related to the bariatric procedure, which equated to 0.02% of total participants). The leading cause of death was sepsis, which is when the immune system produces an extreme response to an infection. Insofar as adverse events were concerned, at 90 days post-surgery, 3.6% of patients had experienced an adverse event such as unplanned readmission, admission to the intensive care unit (ICU), or an unplanned return to the operating theater. More adverse events occurred in revisional procedures than in primary procedures: 55% and 45%, respectively.
“This should reassure patients, their loved ones and payers such as government and insurers that bariatric surgery is safe, effective, and delivers great health improvement,” Brown said. “It will also help to inform more accurate patient consent, so patients have an idea of what they can realistically expect to achieve after an operation and what the risks are.

“The ability to have 61% of people who were being treated for diabetes at the time of their bariatric surgery come off all medications at five years is a major benefit, not just for the individual, but also for our community in terms of health care expenditure.”
That bariatric surgery was found to be safe was of particular significance to the researchers, considering that obesity is traditionally considered a risk factor for anesthesia and other surgical complications.
“The safety of bariatric surgery is reassuring as it means we can safely offer people a way to lose and keep off a substantial amount of weight, offering an opportunity to reverse or improve many health problems,” said Brown. “Usually, they will have tried other ways of losing weight prior to being offered surgery.”
The researchers are planning future research looking at revisional surgery and outcomes in people living with both obesity and diabetes in more detail.
The study was published in the ANZ Journal of Surgery.
Source: Monash University








