New research has identified the mechanism by which air pollution damages the lungs’ self-cleaning system, leaving us vulnerable to infection. In doing so, it has also identified a way to reverse that damage and restore lung function.
We already know that exposure to air pollution is bad for us, and it’s particularly damaging for our lungs. However, what happens at the molecular level to cause that lung damage hasn’t been well known until now.
A new study led by researchers from the Immunology Frontier Research Center (IFReC) at the University of Osaka, Japan, has identified the mechanism by which air pollution damages the airways and, in the process, identified a treatment to potentially reverse it.
“Our results were quite informative,” said lead author Noriko Shinjyo, PhD, an IFReC researcher. “We found that PM2.5 air pollutants negatively affect mucociliary clearance, a major protective mechanism in the respiratory tract. Mucociliary clearance basically involves trapping pollutants in a sticky mucus and then sweeping the pollutants out [of] the airway with hair-like projections called cilia.”
Ciliated cells are lung cells lined with hair-like structures called cilia. As Shinjyo has stated, the cilia play a crucial role in clearing debris from the airways. Each ciliated cell in an airway is equipped with 200 to 300 cilia, the presence of which increases the surface area of these cells to, it’s estimated, hundreds of times higher than that of regular cells. That’s what makes ciliated cells a major point of contact with environmental pollutants.
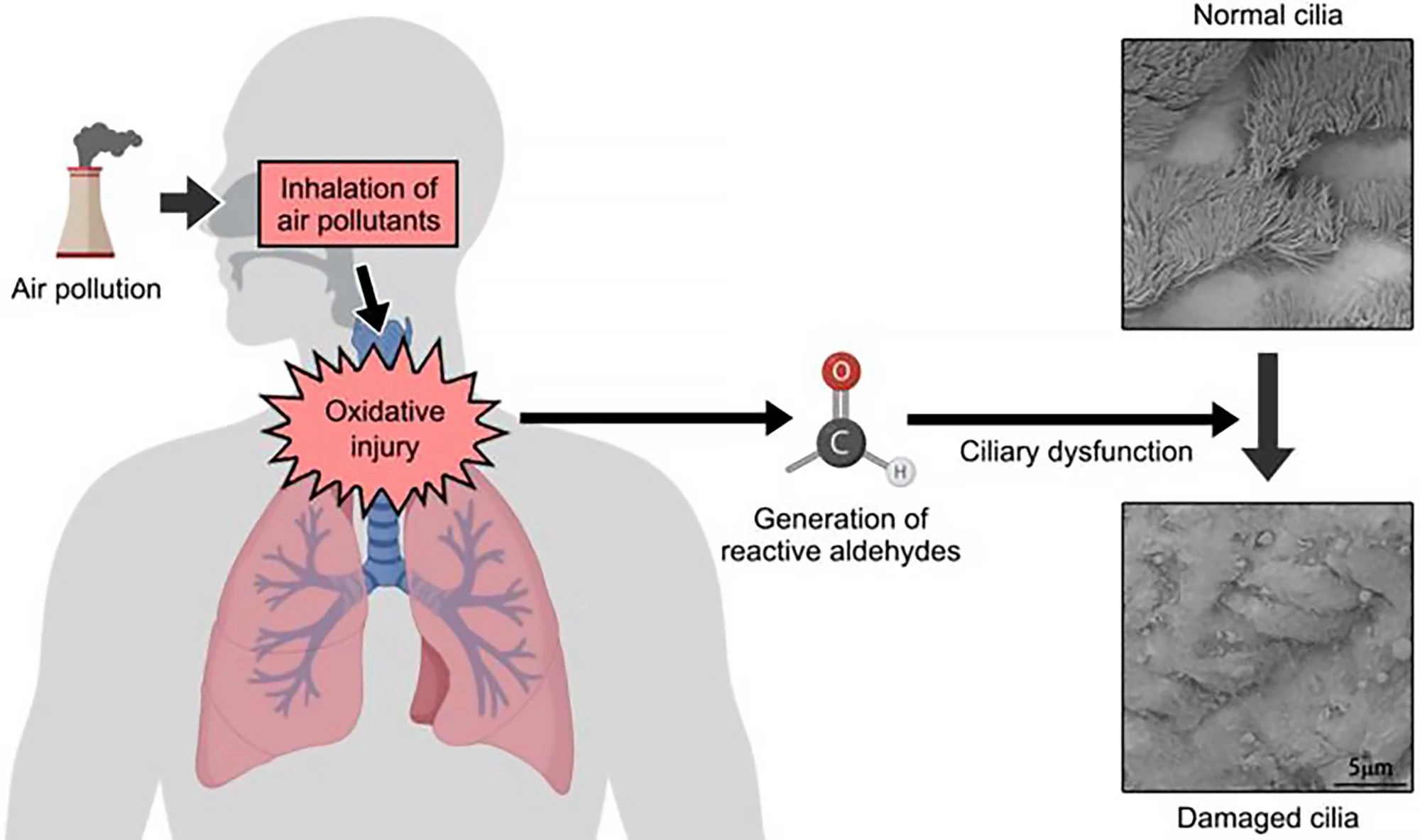
Fine particulate matter, called PM2.5 because its particles are 2.5 micrometers or smaller, commonly comes from natural and human-made sources: cars and truck exhaust, coal-fired power stations, industrial facilities, wildfires and dust storms. Many of these pollutants can generate reactive oxygen species (ROS), leading to oxidative stress that can damage cells and tissues, ultimately resulting in health problems.
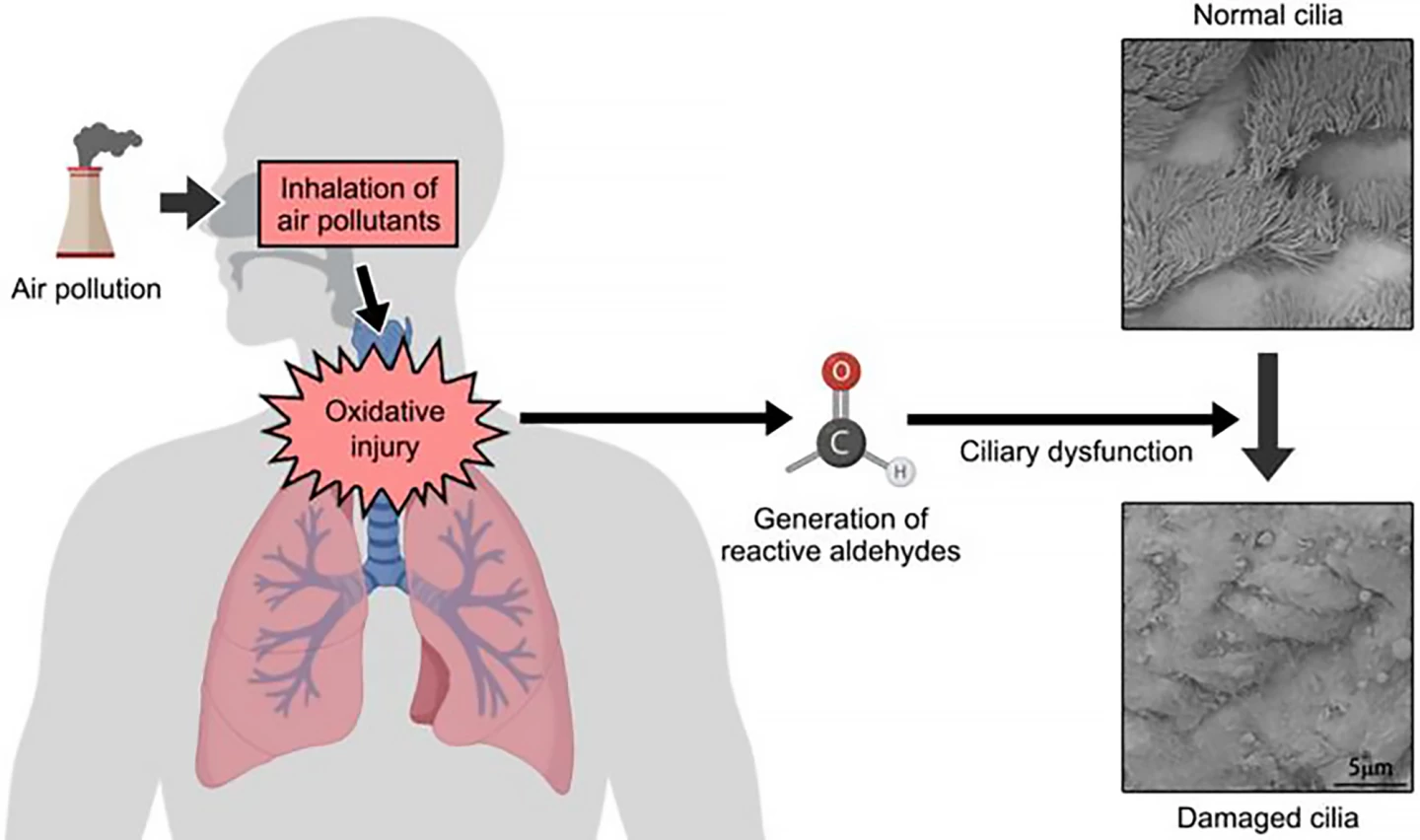
The researchers found that pollutants cause the polyunsaturated fatty acids (PUFAs) found in ciliated cell membranes to undergo oxidation, resulting in the formation of reactive molecules called lipid peroxide-derived aldehydes in the airways. Their reactivity allows them to modify the cells, leading to dysfunction and damage that can extend to the cilia. When they’re damaged, the cells and their attached cilia are less able to move debris out of the lungs, thereby increasing the risk of infection.
Investigating ways to reverse cellular damage and restore normal function, the researchers examined a gene that produces aldehyde dehydrogenase (ALDH1A1), an enzyme involved in breaking down aldehydes.
“Aldehyde dehydrogenase (ALDH1A1) is an enzyme that plays an important role in protection against aldehydes,” said the study’s corresponding author, Yasutaka Okabe, an Associate Professor at IFReC with a particular interest in the mechanisms of airway homeostasis. “We used experimental mice that lacked ALDH1A1 to investigate the impact of air pollutants without the gene. As expected, the mice had impaired cilia formation and function and high levels of aldehydes.”
The mice lacking ALDH1A1 were also at increased risk of developing a serious lung infection when exposed to PM2.5. However, when the researchers administered a drug that increased the mice's ALDH1A1 levels, their mucociliary function was restored.
“Altogether, these results demonstrate aldehyde metabolism ensures ciliary resilience and illuminates its therapeutic potential in mitigating respiratory disorders associated with air pollution,” the researchers said.
Future research will investigate the impact of aldehyde metabolism in other respiratory diseases, including asthma, chronic obstructive pulmonary disease (COPD), and cystic fibrosis, which have also been linked to PM2.5 exposure.
The study was published in the Journal of Clinical Investigation.
Sources: IFReC, EurekAlert!