A coughing, sneezing, 3D-printed model of the human nose and upper airway has provided researchers with a better understanding of how airborne infections are transmitted. The knowledge will aid in developing effective ways of reducing that spread.
The global COVID-19 pandemic demonstrated how easily respiratory diseases can be spread through coughing and sneezing. Accurately replicating airborne disease transmission is essential for understanding how respiratory diseases are spread. However, it’s not always possible to recruit sick people for studies.
To that end, researchers from the Universitat Rovira i Virgili (URV) in Spain have designed and built a 3D model of the human upper airway and nasal cavity that is capable of simulating coughing and sneezing to better study the spread of disease-carrying particles.
“This novel experimental setup is used here to generate exhalations resembling human coughs and sneezes with adjustable parameters used to control the air ejection strength,” said the researchers. “Using realistic three-dimensional (3D) printed models of the upper respiratory tract and nasal cavity, we can investigate the role of the exhalation strength and the role of nasal airways (by blocking or not the nostrils of the model) on the aerosol cloud dispersion.”
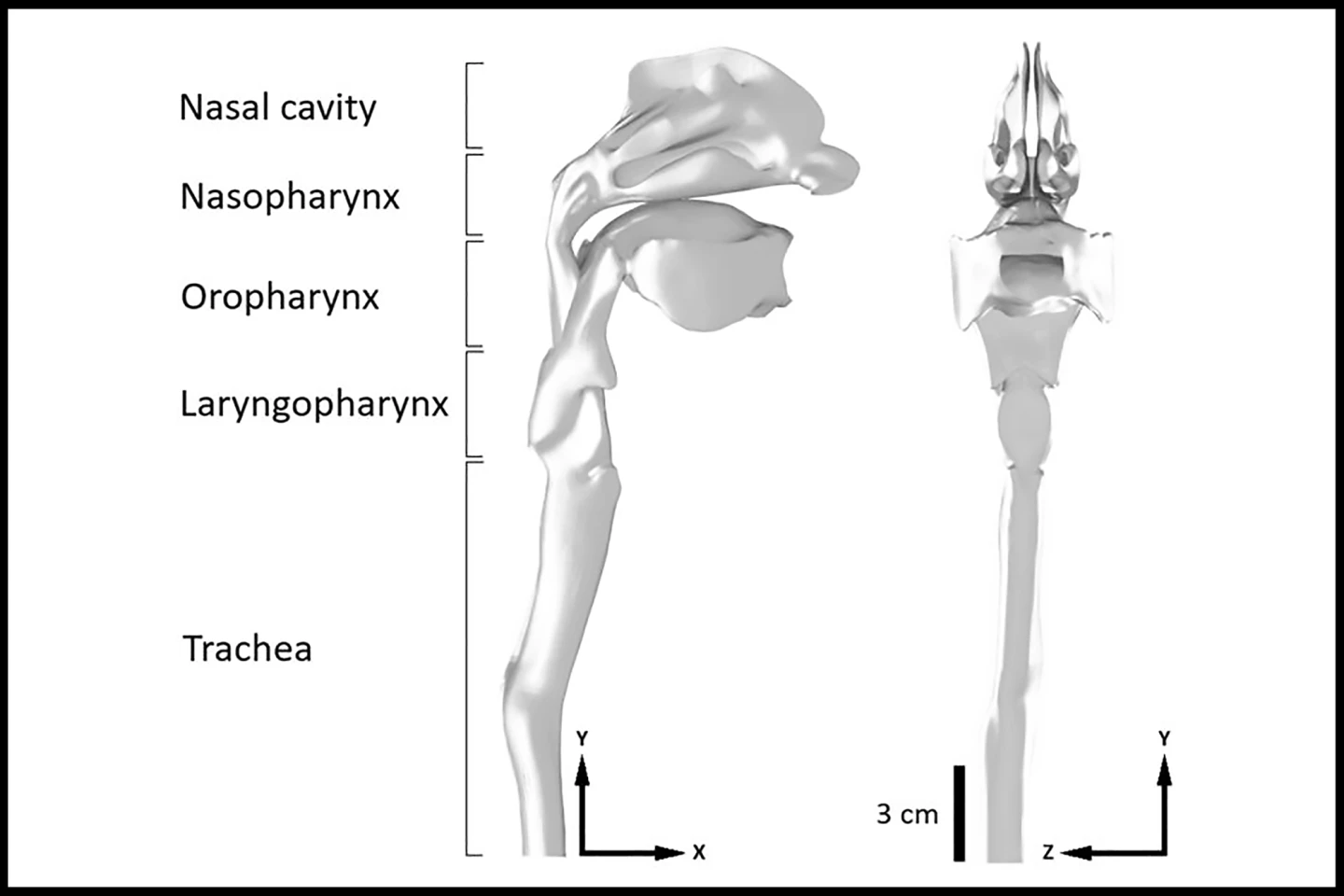
The nasal cavity is crucial to airflow dynamics and the size, direction, and dispersion rate of particles expelled during a cough or sneeze. There are also differences between particles expelled through the nose or mouth. Because these factors impact disease transmission, the researchers wanted to design a respiratory model that was as true to life as possible.
The researchers used high-speed cameras and a laser beam to study how air particles dispersed in the air in real-time. They measured particle cloud trajectory and width under a range of experimental conditions designed to mimic different “violent expiratory events” through the nose or mouth.
The researchers found that exhaling through the nose caused infectious particles to be deflected downward, dispersing them more vertically and less horizontally. They say that while this may reduce the risk of disease transmission to people in the immediate vicinity, it also means that particles are suspended in the air for longer. In confined spaces with poor ventilation, this can increase the risk of exposure to others in the long term.
In contrast, exhaling through the mouth caused infectious particles to travel further, along a more horizontal path. This dispersal pattern, the researchers say, increases the risk of infection spread to people in close proximity, as particles are likely to land directly on them, especially during face-to-face conversations or in shared environments.

“These results help us to understand how particle nuclei are dispersed in indoor spaces and, consequently, how diseases are transmitted through the air,” said Nicolás Catalán, a researcher at URV’s Department of Mechanical Engineering and the study’s lead author.
While further study is needed to examine how environmental factors such as humidity and temperature affect particle dispersion, the understanding gleaned from the present study can inform ventilation strategies in restaurants, classrooms, hospitals, public transport, and the like.
“Optimizing ventilation systems based on particle cloud dynamics has the potential to significantly reduce the risk of airborne disease transmission,” the researchers said.
The study was published in the journal Physics of Fluids.
Source: Universitat Rovari i Virgili








