A team of researchers have developed a 3D-printed, biodegradable heart patch that seals holes in heart tissue and supports tissue regeneration, showing promise as a safer alternative to current surgical materials.
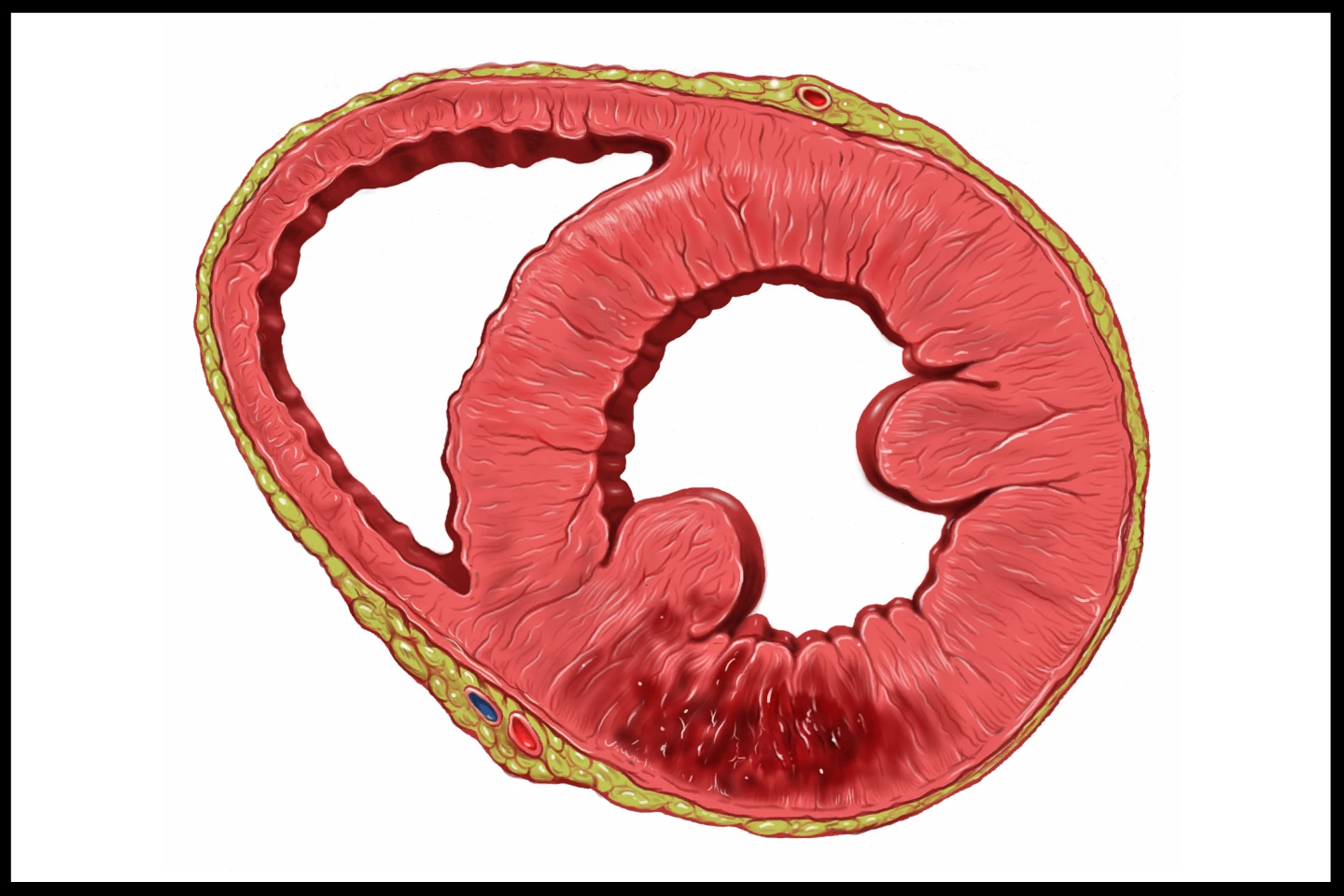
Worldwide, the leading cause of death is heart attack. Those who survive a heart attack face an ongoing issue with the heart’s efficiency, caused by the death of heart cells and the scar tissue that subsequently forms. In severe cases, the heart wall can rupture, requiring emergency surgery.
Over the years, scientists have developed implantable patches to seal and support damaged heart tissue. In a new study led by ETH Zurich in Switzerland, researchers developed and tested a new type of cardiac patch that not only seals defective areas of the heart, but also heals them.
“Traditional heart patches do not integrate into the heart tissue and remain permanently in the body,” said the study’s lead author, Lewis Jones, a bioengineering researcher at ETH Zurich’s Soft Robotics Lab. “We wanted to solve this problem with our patch, which integrates into the existing heart tissue.”
“Our goal was to develop a patch that not only closes a defect but also helps to repair it completely,” added corresponding author Professor Robert Katzschmann, PhD, who’s also from the Soft Robotics Lab.
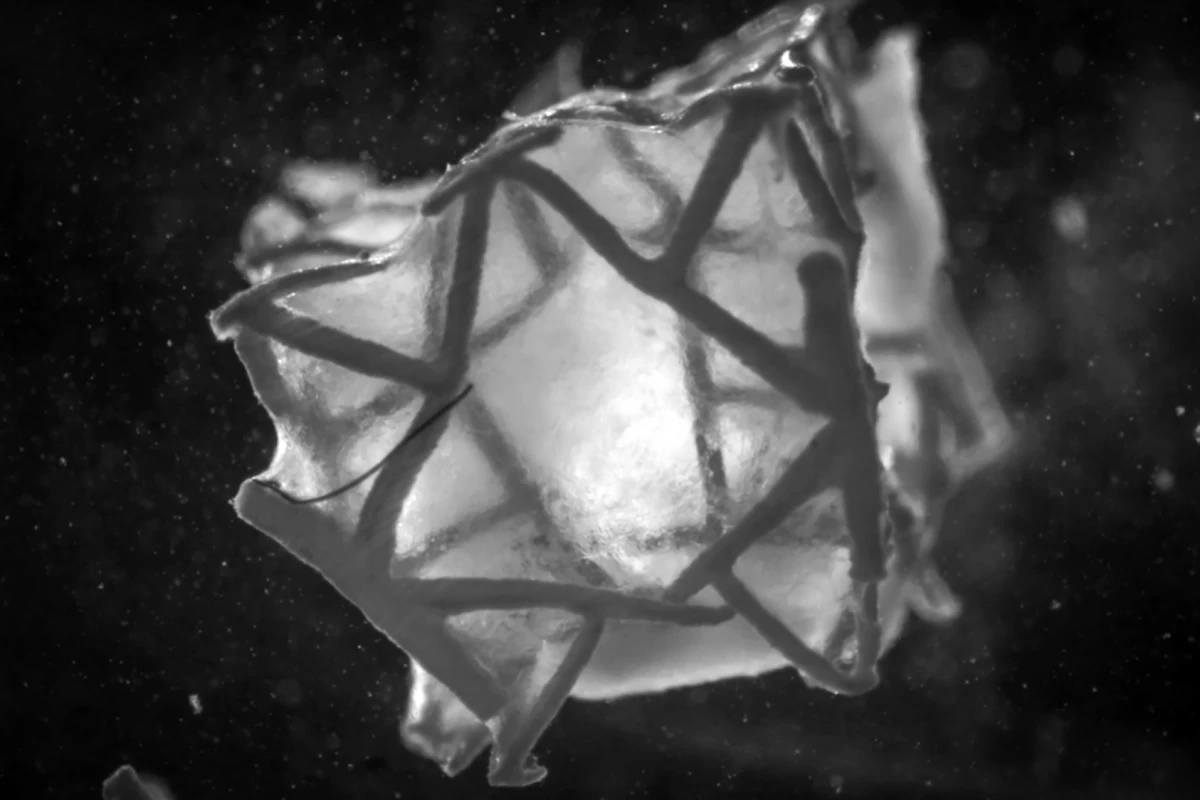
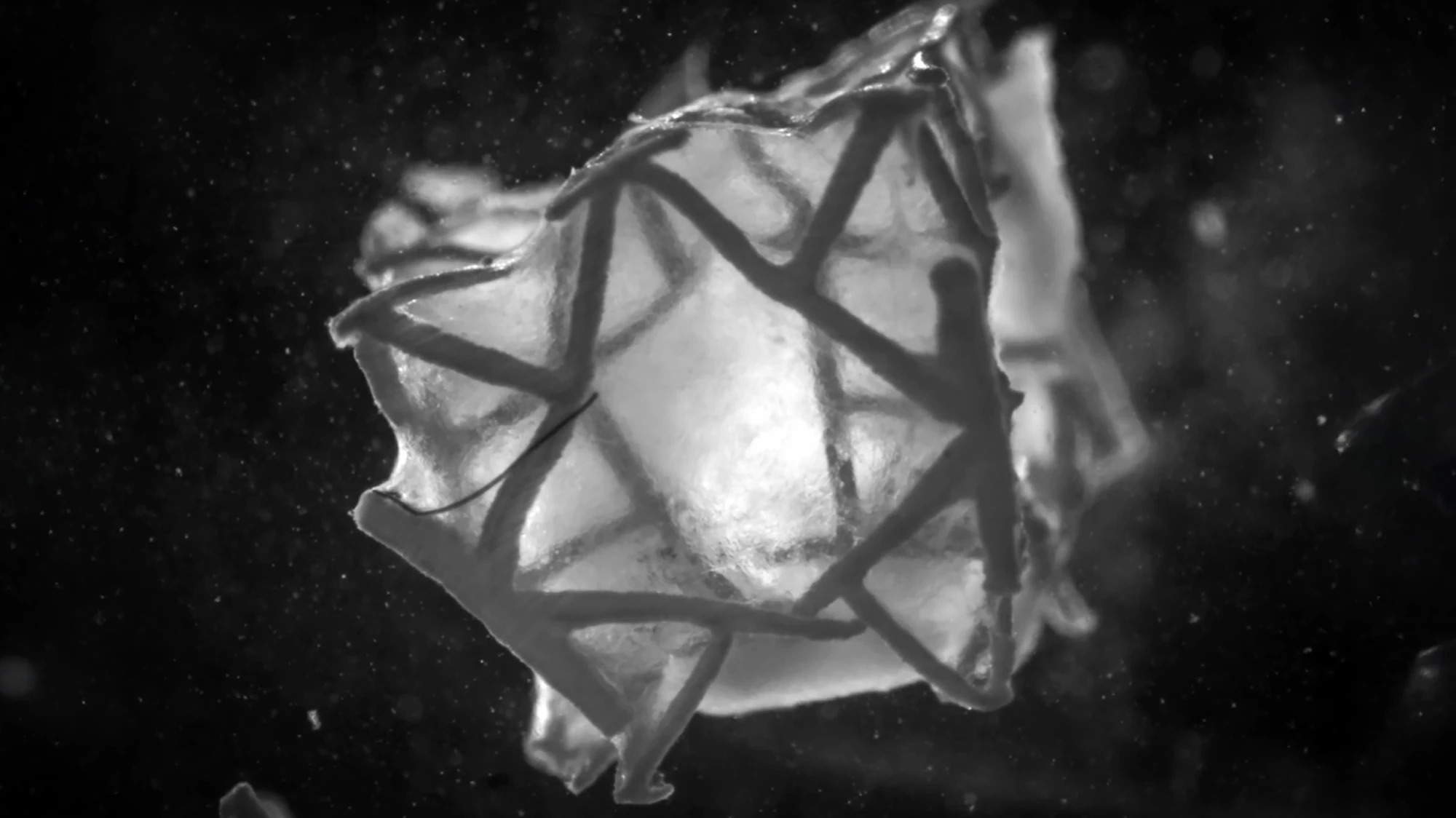
To create their implantable, reinforced cardiac tissue patch, which they called the “RCPatch,” the researchers 3D printed a biodegradable, biocompatible polyester metamaterial scaffold with tunable stiffness, meaning its rigidity or flexibility could be adjusted to match surrounding heart tissue. However, they didn’t just come up with a structure out of thin air; they used generative computer modeling and computer simulations to design hundreds of potential 3D lattice structures, before they selected one with mechanical properties similar to the heart’s.
The scaffold was infused with a fibrin-based hydrogel containing induced pluripotent stem cell-derived cardiomyocytes (iPSC-CMs), which is just science-speak for heart muscle cells that have been lab-grown from adult cells like skin cells. A mesh was added that was separately infused with fibrin hydrogel to reduce blood leakage and provide a suturable surface that could be attached surgically.
“The scaffold is stable enough and can be filled with a hydrogel containing living cells,” said Jones. “The big advantage is that the scaffold is completely degraded after the cells have combined with the tissue. This means that no foreign body remains.”
The RCPatch was cultured in the lab until the heart cells began contracting, which occurred within about three days. The researchers then assessed the patch’s durability under repeated stretching and compression for up to thousands of cycles, to mimic heartbeats. The final step was implanting the patch over an 8-mm (0.3-in) hole in the left lower chamber (left ventricle) of a pig’s heart.
If you’re okay with watching bloody, real-life surgical procedures, check out the video below, which shows the researchers attaching the proof-of-concept patch and watching it work. You can see that after the patch is attached to the still-beating heart, bleeding from the ventricular hole stops almost immediately. Minor bleeding continued for about 10 minutes.
“We were able to show that the patch retains its structural integrity even under real blood pressure,” said Katzschmann.
The major limitation of the study is that it was an early-stage proof-of-concept that was only tested in one animal, and only in the short term. Additionally, in the real world, holes left by ruptured ventricles can be larger and more irregular than the 8-mm ventricular hole that the patch covered. It’s unknown how the patch degrades, integrates, or supports functional heart recovery over weeks or months.
Nonetheless, with further development and validation, the RCPatch could be a biodegradable, regenerative alternative to animal-derived heart patches, enabling ventricular repairs and improving outcomes. It has the potential to decrease the risk of serious, long-term complications associated with heart attacks.
The study was published in the journal Advanced Materials.
Source: ETH Zurich