For the first time, scientists have combined the six primary skin cell types with specialized hydrogels to ‘print’ a thick, multilayered skin that, when transplanted, successfully integrated with surrounding tissue to heal wounds faster and with less scarring.
“Comprehensive skin healing is a significant clinical challenge, affecting millions of individuals worldwide, with limited options,” said lead author Dr Anthony Atala, director of Wake Forest Institute for Regenerative Medicine (WFIRM). “These results show that the creation of full thickness human bioengineered skin is possible and promotes quicker healing and more naturally appearing outcomes.”
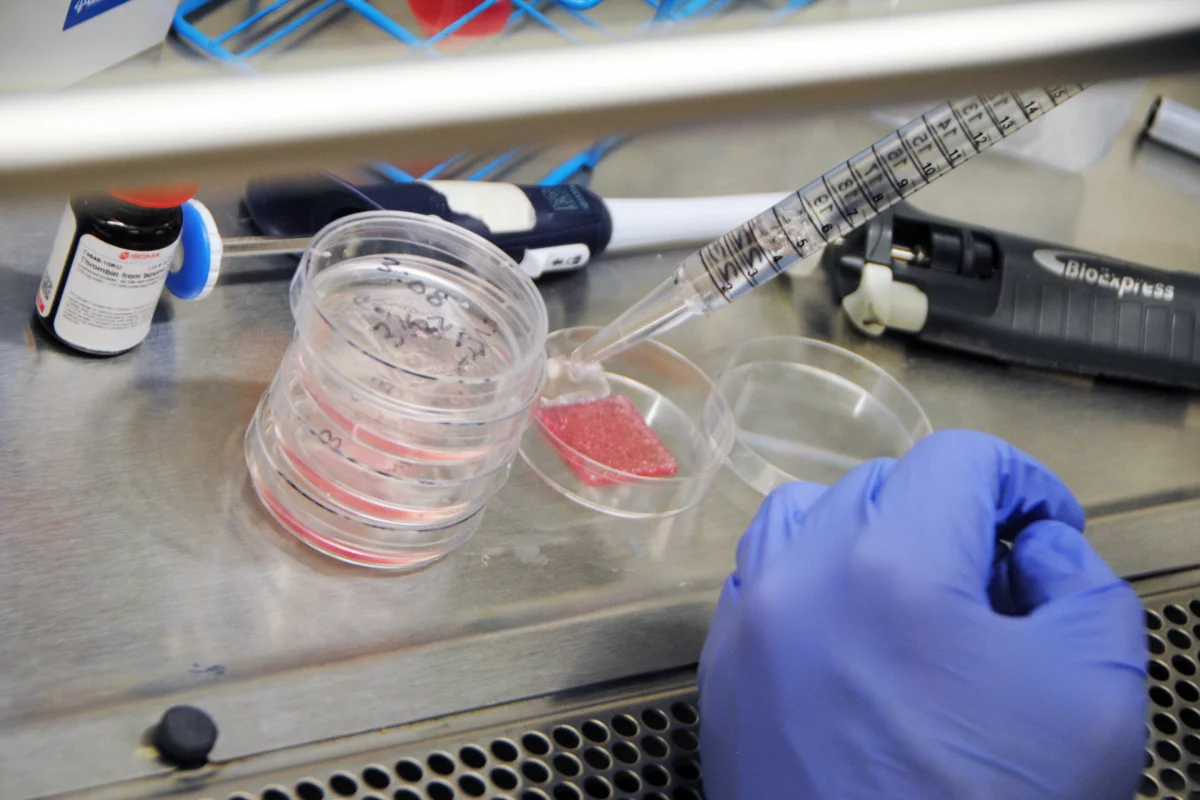
The printed skin, which features keratinocytes, dermal fibroblasts, adipocytes, melanocytes, follicle dermal papilla cells and dermal microvascular endothelial cells, replicated the real thing, with three layers: the thin, protective outer epidermis, the middle fibrous and supportive dermis and the bottom, fatty hypodermis.
When transplanted onto mice wounds, the printed skin formed blood vessels, skin patterns and showed normal tissue development. The result was quicker wound closure, less skin contraction and more collagen production, resulting in less scarring. With cell-specific staining, the WFIRM team confirmed the successful integration of the bioprinted cells with the regenerated skin during the healing process.
Following this, the researchers used a larger, 5-cm x 5-cm (2-in x 2-in) bioprinted porcine skin graft to cover a full-thickness wound on a pig model. Similarly, it improved healing and collagen production, and reduced skin contraction and fibrosis (or scarring).
The success of the larger, autologous graft shows great promise in human therapeutics, where harvesting substantial amounts of skin from other areas of the body is risky and limited.
Lab-made skin is a growing area of medical research, and companies are also looking to it to test products instead of using animals. But this is the first time a product of this complexity and thickness has been produced that has shown complete wound healing in pre-clinical studies. The team is now hopeful of its development for human study.
The research was published in the journal Science Translational Medicine.