Blood stem cell donation is an important medical procedure, but it’s subject to constant shortages. Researchers at the University of New South Wales (UNSW) have now demonstrated how a microfluidic device that mimics the embryonic heart can produce blood stem cell precursors, which could let blood stem cells be manufactured on demand.
As with organs and regular blood transfusions, patients receiving donated blood stem cells need to have the same blood type as their donor to prevent their immune system rejecting the foreign cells. That leads to shortages of viable donors, especially for rarer blood types.
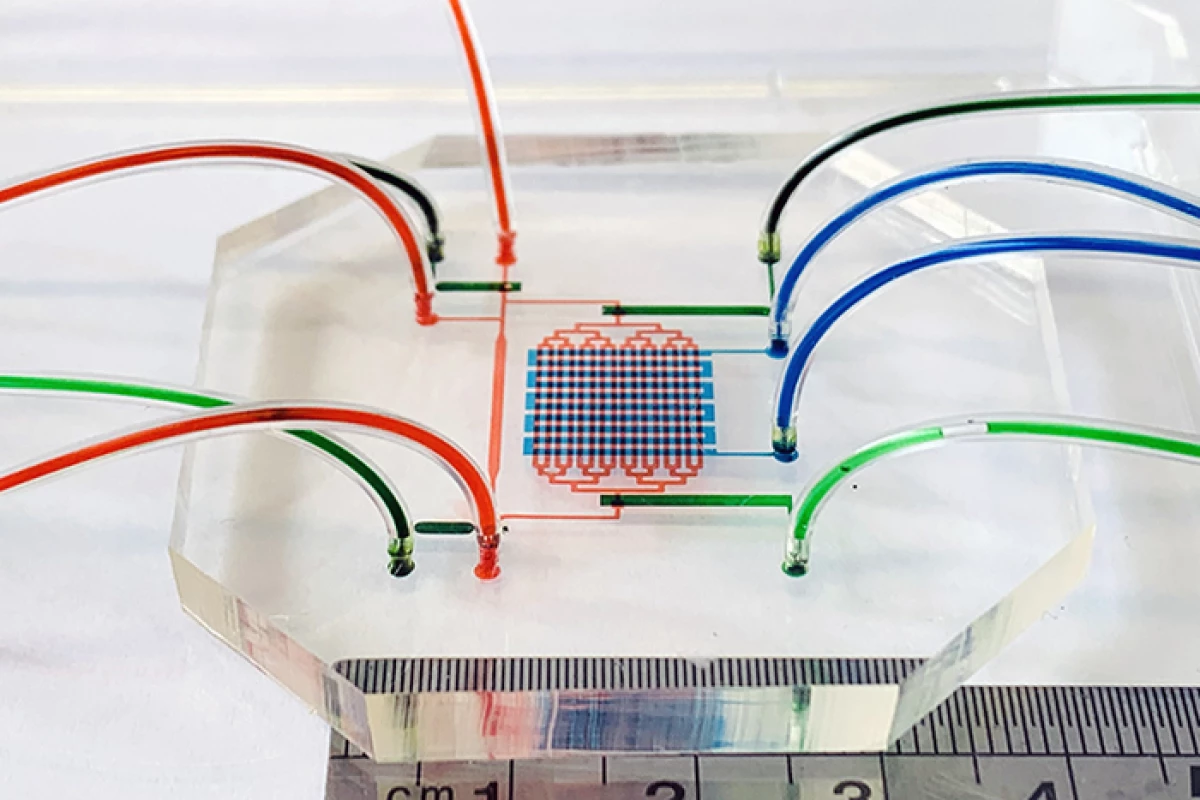
Ideally, scientists would be able to grow blood stem cells in the lab, which could theoretically be given to whoever needs them. This could be done by cultivating precursor cells, which themselves can differentiate into a variety of cell types, including red and white blood cells. For the new study, the UNSW team investigated this idea using a microfluidic device that pumped blood stem cells taken from an embryonic stem cell line.
“Part of the problem is that we still don’t fully understand all the processes going on in the microenvironment during embryonic development that leads to the creation of blood stem cells at about day 32,” said Dr. Jingjing Li, lead author of the study. “So we made a device mimicking the heart beating and the blood circulation and an orbital shaking system which causes shear stress – or friction – of the blood cells as they move through the device or around in a dish.”
And sure enough, the device was found to promote the development of precursor blood stem cells. Not only that, but these precursors also went on to produce differentiated blood cells, and even cells like those that line the blood vessels, which are responsible for creating the blood stem cells in the developing embryo.
“Getting an aorta to form and then the cells actually emerging from that aorta into the circulation, that is the crucial step required for generating these cells,” said Robert Nordon, co-author of the study. “What we've shown is that we can generate a cell that can form all the different types of blood cells. We've also shown that it is very closely related to the cells lining the aorta – so we know its origin is correct – and that it proliferates.”
The team hopes this work could eventually lead to devices that can incubate large batches of blood stem cells, which would reduce the reliance on donors and cut wait times. The researchers are currently working on upscaling the technique using bioreactors to cultivate the cells.
The research was published in the journal Cell Reports.
Source: UNSW