Autoimmune diseases affect almost four percent of the global population, the most common being Crohn’s disease, psoriasis, multiple sclerosis, and rheumatoid arthritis. A new study has identified a naturally occurring compound that may provide a new way of treating these debilitating diseases.
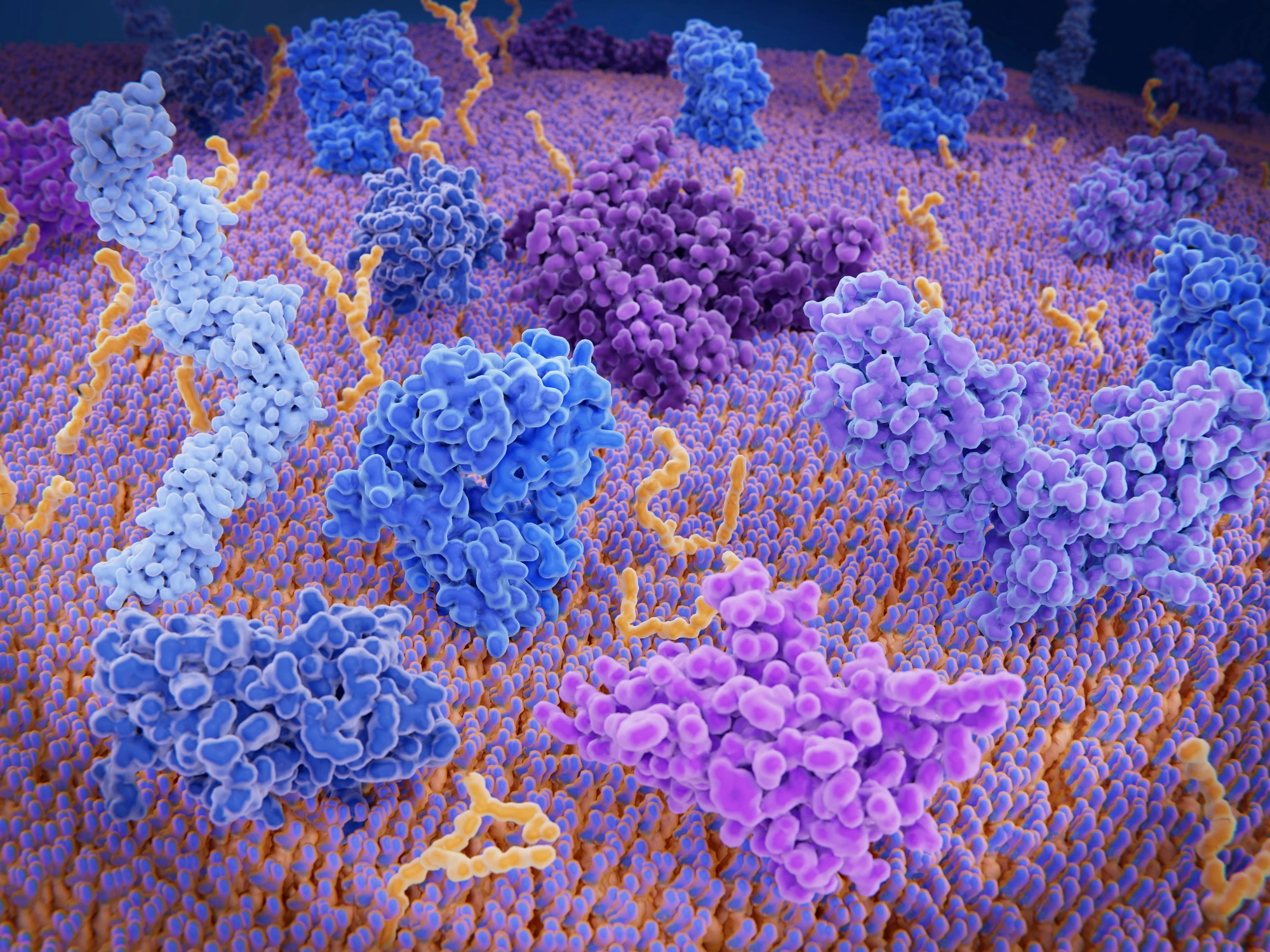
T cells are key to the body’s immune response, attacking pathogens and infections. In autoimmune diseases, the immune response is faulty, and the T cells start attacking healthy cells and tissues, but the mechanism underlying this is poorly understood.
Our adaptive immune system responds to particular pathogens we encounter, creating a long-lasting "memory" so the body knows how to fight that pathogen should we encounter it again. T helper (Th) cells are a type of T cell that plays a central role, releasing cytokines that activate other immune cells to fight invading pathogens.
One cytokine important to the body’s inflammatory response, interleukin 17 (IL-17), is secreted by a subtype of Th cells called Th17 cells. Th17 cells bolster the immune response, causing an accumulation of immune cells at inflammatory sites. But, when they’re overactivated, they can attack healthy cells, leading to autoimmunity.
A new study out of Japan focused on the role that Th17 cells play in autoimmune diseases. Researchers started by looking at glycolysis, the metabolic process by which glucose is converted into energy to fuel cells, which is also responsible for creating Th17 cells.
“What’s interesting is that excessive glycolysis seems to suppress Th17 cell activity,” said Tsung-Yen Huang, the study’s first author. “So, we hypothesized that molecules produced during glycolysis may inhibit the cells.”
Glycolysis produces a byproduct called phosphoenolpyruvate (PEP). The researchers discovered that introducing additional PEP into the cells prevented Th17 cells from maturing and inhibited IL-17 production, thereby reducing the body’s inflammatory response. Importantly, adding PEP to the cells did not greatly affect the glycolytic process or T cell activation.
Delving deeper into the process underpinning PEP’s inhibitory action, they found that a protein called JunB promoted Th17 maturation by binding to a specific set of genes. Further experimentation showed that PEP treatment blocked JunB activity, inhibiting the creation of Th17 cells.
Testing what they’d discovered on mice with an autoimmune brain disease, the researchers found that daily administration of PEP stopped the generation of Th17 cells and reduced the Th17-dependent autoimmune response.
“The key to the development of autoimmune diseases, and thus the way to inhibit this development, lies in our cells, but the underlying mechanism has always been unclear,” said Professor Hiroki Ishikawa, corresponding author of the study. “Now, our research has shed light on a compound that could suppress the development of these diseases.”
This study could present a novel way of treating autoimmune diseases without interfering with the important metabolic process of glycolysis. The researchers are keen to improve the process before proceeding to human clinical trials.
“Our results show the clinical potential of PEP," Huang said. "But first, we need to increase its efficiency.”
The study was published in the journal Cell Reports.