Believed to be caused by a mix of genetic and environmental factors, Parkinson’s disease is a chronic, progressive disease that affects the central nervous system, particularly the motor system, resulting in tremors, rigidity, and difficulty walking. New research has found that a gene associated with an increased risk of Parkinson’s disease also contributes to one of the hallmarks of the disease.
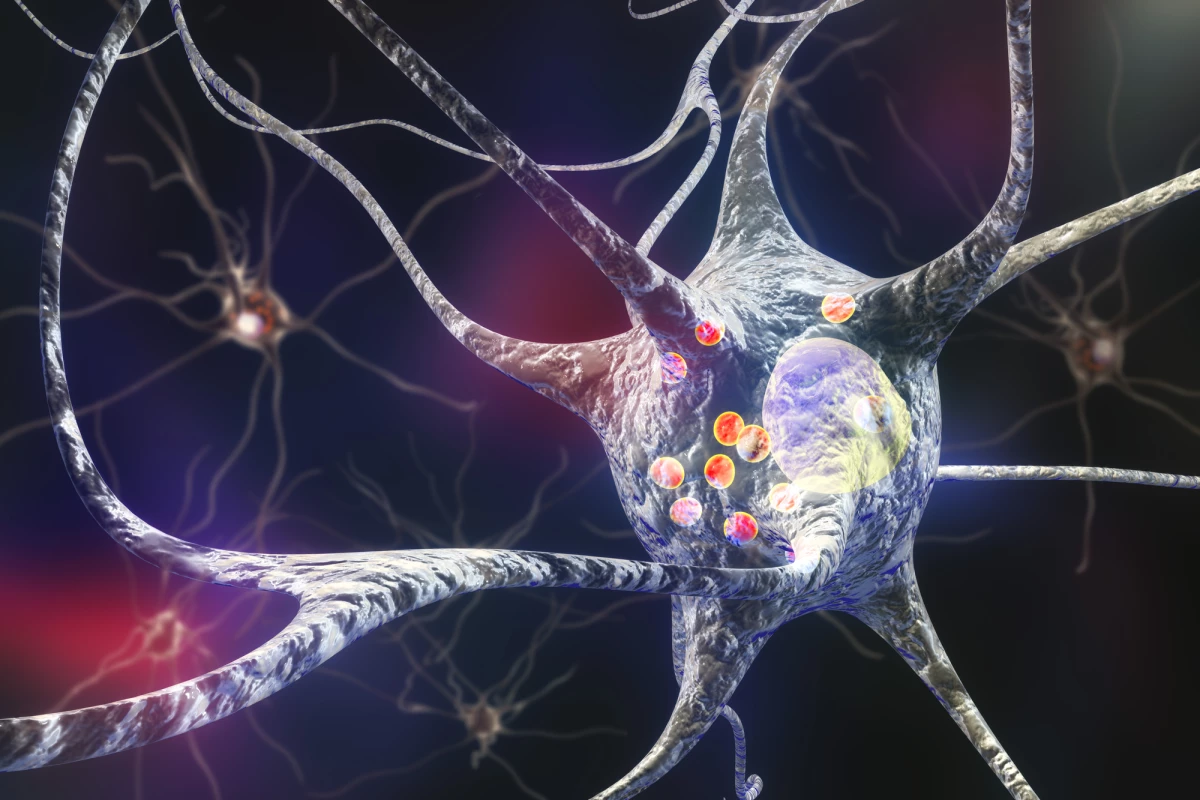
At the end of of the part of a nerve cell called an axon sits the pre-synaptic terminal. Here, a nerve impulse is converted into a neurotransmitter, which carries the signal across the synapse between two neurons or between a neuron and a muscle cell or gland.
Synapses are densely packed with proteins that fuel the metabolic activity that takes place there. They are also fragile structures. The intensity of metabolic activity required to maintain neurotransmission can stress and damage cells. If the damaged cells are not cleared by a process known as autophagy, it can result in a toxic build-up of cellular debris and the death of neurons, both of which are seen in Parkinson’s disease.
A new study by the University of Queensland in Australia examined how dysfunctional autophagy contributes to neuronal degeneration. The researchers were aware that when cells broke down, they signaled the production of a protein called Endophilin-A (EndoA) to start the clean-up of cellular debris in the brain.
“We knew we could induce autophagy in cells by starving them of amino acids and the subsequent breakdown of debris tells a protein called EndoA to approach the cell membrane and begin the recycling process,” said Dr Adekunle Bademosi from the Queensland Brain Institute and lead author of the study.
Their research led to the discovery of a gene mutation that is associated with an increased risk of Parkinson’s disease and the build-up of cellular debris in the brain.
“Our team has found that a Parkinson’s disease-linked mutation in a gene called Endophilin-A1 blocks the process by which the body and the brain recycle cell waste,” Bademosi said.
“Unfortunately, when the Endophilin-A1 gene is affected in Parkinson’s, the protein EndoA becomes insensitive to this trigger at the synapse and the debris that should be thrown out for recycling builds up instead,” he added.
The study's results suggest a move away from traditional treatments for Parkinson’s disease, focusing instead on addressing the build-up of cellular debris that may underlie the condition.
“It may be time to shift the treatment focus to autophagy as the mechanism underlying these disease hallmarks,” Bademosi said. “Exploring the use of compounds that induce or inhibit autophagy could pave the way for new, more effective Parkinson’s drugs.”
The study was published in the journal Neuron.
Source: University of Queensland