Ordinarily, when treating chronic wounds, caregivers go to great lengths to keep them free of bacteria. An experimental new dressing, however, actually introduces bacteria to help such wounds heal.
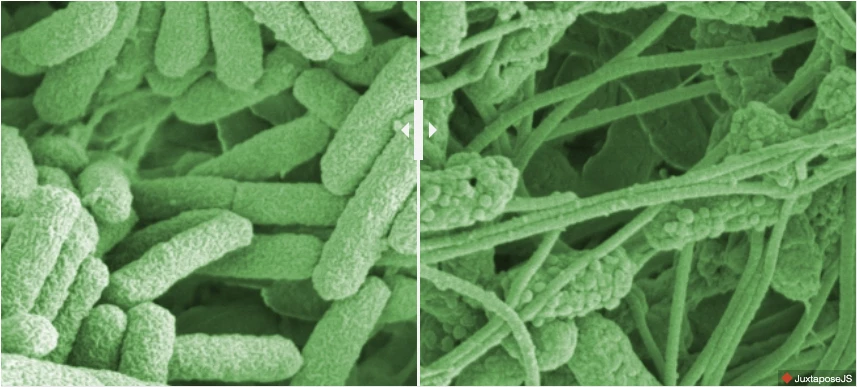
When a diabetic skin ulcer or other chronic wound becomes infected, colonies of the problematic bacteria within it form a layer of mucus known as a biofilm. This film largely protects the microbes from the antibacterial effects of antibiotics or disinfectants.
Seeking a method of destroying these biofilms at the wound site, scientists from MIT and Switzerland's Empa research institute looked to an existing product known as Bio-K+. Marketed primarily as a gut health supplement, it contains three types of lactobacilli probiotic bacteria.
The scientists added Bio-K+ to a commercially available hydrogel wound dressing called Aquacel, then applied the augmented dressing to a biofilm culture produced by Pseudomonas aeruginosa bacteria (one of the main culprits in wound infections). As the lactobacilli in the dressing produced lactic acid, they caused the pH of the biofilm to drop to an acidic level, thus destroying it.
Next, the dressing was applied to small wounds made in human skin samples on which P. aeruginosa biofilms had grown. The dressing killed 99.999% of the pathogens, while not harming any skin cells. And as an added bonus, the probiotic bacteria also promoted fibroblasts – which are cells that contribute to the formation of connective tissue – to migrate into the wounds.
A paper on the research, which was led by Empa's Dr. Qun Ren, was recently published in the journal Microbes and Infection.
Source: Empa




