Could the future of rheumatoid arthritis treatment be a small implant designed to deliver bursts of electrical stimulation to a key nerve that can regulate the body’s inflammatory reflex? A flurry of research around the world is investigating this compelling idea, with large-scale clinical trials underway testing several kinds of novel implants.
Running from the brainstem down to the abdomen through the neck and chest, the vagus nerve is a large conduit that communicates signals between the brain and the body. Electrically stimulating this nerve using small implants is already approved by the US Food and Drug Administration (FDA) to treat some forms of epilepsy and depression.
Plus, a great deal of research has focused on how the vagus nerve mediates communication between the gut and the brain. This has led to the development of small devices designed to suppress a person’s appetite by gently stimulating the vagus nerve, tricking the brain into thinking the gut is full.
More recently, researchers have discovered yet another role of the vagus nerve – communicating to the brain when the body is experiencing inflammation. The research has revealed the vagus nerve can act as a brake for the immune system, sending signals to the spleen slowing down its release of inflammatory molecules.
Last year, the results of the first in-human pilot study testing a vagus nerve stimulation device for rheumatoid arthritis were published. The study was small but the results were promising, with no device-related or treatment-related serious adverse events. And, more importantly, the treatment reduced signs and symptoms of rheumatoid arthritis in the small cohort.
The world’s first large-scale Phase 3 trial testing this experimental arthritis therapy kicked off this year. Set to recruit 250 subjects, spanning 40 sites across the United States, the trial will be the first to robustly test whether vagus nerve stimulation can treat this common auto-immune disease.
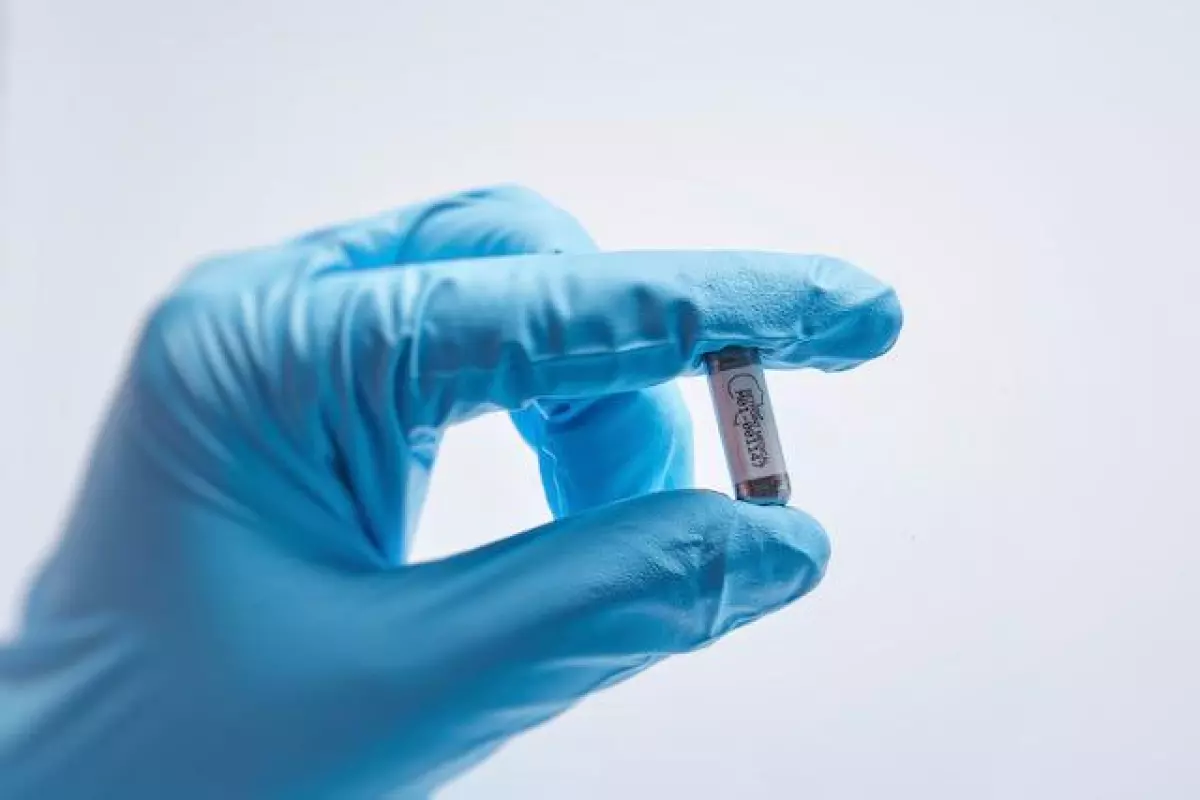
Andrew Ko, a neurosurgeon from the University of Washington, says the device being tested in the trial is about the size of a vitamin tablet and it's surgically inserted through a small incision in the neck. The implant can be recharged wirelessly by wearing a small collar-like device for an hour each week.
The trial will be blinded and placebo-controlled, with half the cohort randomly assigned to a placebo group that will receive the surgical implant but not be administered any electrical stimulation. And the stimulation being tested will only consist of one minute of activation per day.
“These low-voltage stimulations will be administered at night while patients are asleep, so they won’t even notice it,” explains Ko.
The trial is set to last around three years to account for long-term safety and efficacy data. However, the active intervention period will only span 12 weeks. Ko also says if the trial is successful this specific implant will be tested on other autoimmune diseases.
“Rheumatoid arthritis was chosen to study because it is well characterized and there are established ways to track its severity but if this novel approach proves effective, it may work for other autoimmune diseases as well,” explains Ko.
We’re working towards the day when people with rheumatoid arthritis won’t have to remember to take medication every day and won’t have to cope with side effects
A team in Australia, from the non-profit research organization Bionics Institute, is also working on a vagus nerve stimulation device for rheumatoid arthritis. This device is a little different from the one being trialed in the United States.
The Australian device is implanted via keyhole surgery into the stomach, targeting several spots on the vagus nerve in the abdomen. The developers of the device say stimulating this particular part of the nerve allows for more targeted responses in the spleen, avoiding some potential adverse effects on the heart or lungs that may be seen when the vagus nerve is stimulated higher up.
The device is connected to a battery that is implanted around the hip. Robert Klupacs, CEO of the Bionics Institute, says the battery should last around 10 years, meaning the implant is “set and forget” as it needs no weekly charging.
“We’re working towards the day when people with rheumatoid arthritis won’t have to remember to take medication every day and won’t have to cope with side effects,” says Klupacs. “They can ‘set and forget’ about this electrical vagus nerve device, leaving their body to do the work for them.”
The Bionics Institute device was originally developed to treat Crohn’s disease, a type of inflammatory bowel disease, and clinical trials are already underway testing the the efficacy of the device in this condition.
Most recently a study published in The Lancet reported a successful proof-of-concept pilot study testing a non-invasive vagus stimulation device for rheumatoid arthritis. This device, worn behind the ear, delivers mild electrical stimulation to the vagus nerve for up to 30 minutes a day.
The majority of the cohort in the pilot study showed clinically significant improvements at the end of the 12-week trial. Almost one quarter of the cohort of 27 achieved disease remission by the end of the study. Future trials with a placebo group will be needed to validate these findings.
It is still early days for the field of study investigating how electrical stimulation of the vagus nerve can influence inflammation and plenty of questions still remain unanswered: What autoimmune diseases could this kind of biostimulation work for? What is the best way to deliver this therapy? Can the vagus nerve be effectively stimulated non-invasively or will a surgical implant ultimately be necessary?
Despite the work ahead, the potential for this novel anti-inflammatory treatment is immense. Evange Romas, a rheumatologist working with the Bionics Institute team in Australia, says it's hard to overstate the potential life-changing effects if this kind of therapy works. With current arthritis treatments often generating harsh side effects – if they even work in the first place – a simple electrical implant regulating inflammation in the body could be a game-changing innovation.
“I have been involved in some great advances in the treatment of rheumatoid arthritis during my career," says Romas. "However, this new treatment is incredibly exciting and I’m doing everything in my power to help the Bionics Institute researchers get it into the clinic for the benefit of my patients as soon as possible.”