A new nanoparticle drug has shown preclinical promise in both preventing rheumatoid arthritis and reducing painful flare-ups, offering hope for a targeted, steroid-sparing treatment that calms the immune system without widespread suppression.
Disease-modifying anti-rheumatic drugs, or DMARDs, have advanced the treatment of the chronic autoimmune disease rheumatoid arthritis (RA), with about half of patients achieving remission or low disease activity in the form of reduced inflammation and slowed joint damage.
Now, in a new study, researchers have tested a new type of nanoparticle-based drug, called Agg-CLNP, to improve the prevention of RA and reduce flare-ups in people who already have the disease.
They created the nanoparticles from biodegradable polymers and coated them with aggrecan (that’s where the Agg in the drug’s name comes from). This peptide is primarily found in cartilage and plays a crucial role in its ability to withstand compressive forces. In RA, the breakdown of aggrecan is one of the earliest events leading to cartilage damage. The nanoparticles were loaded with calcitriol, the active form of vitamin D3; hence, the CLNP part of the drug’s name: calcitriol-loaded nanoparticles.
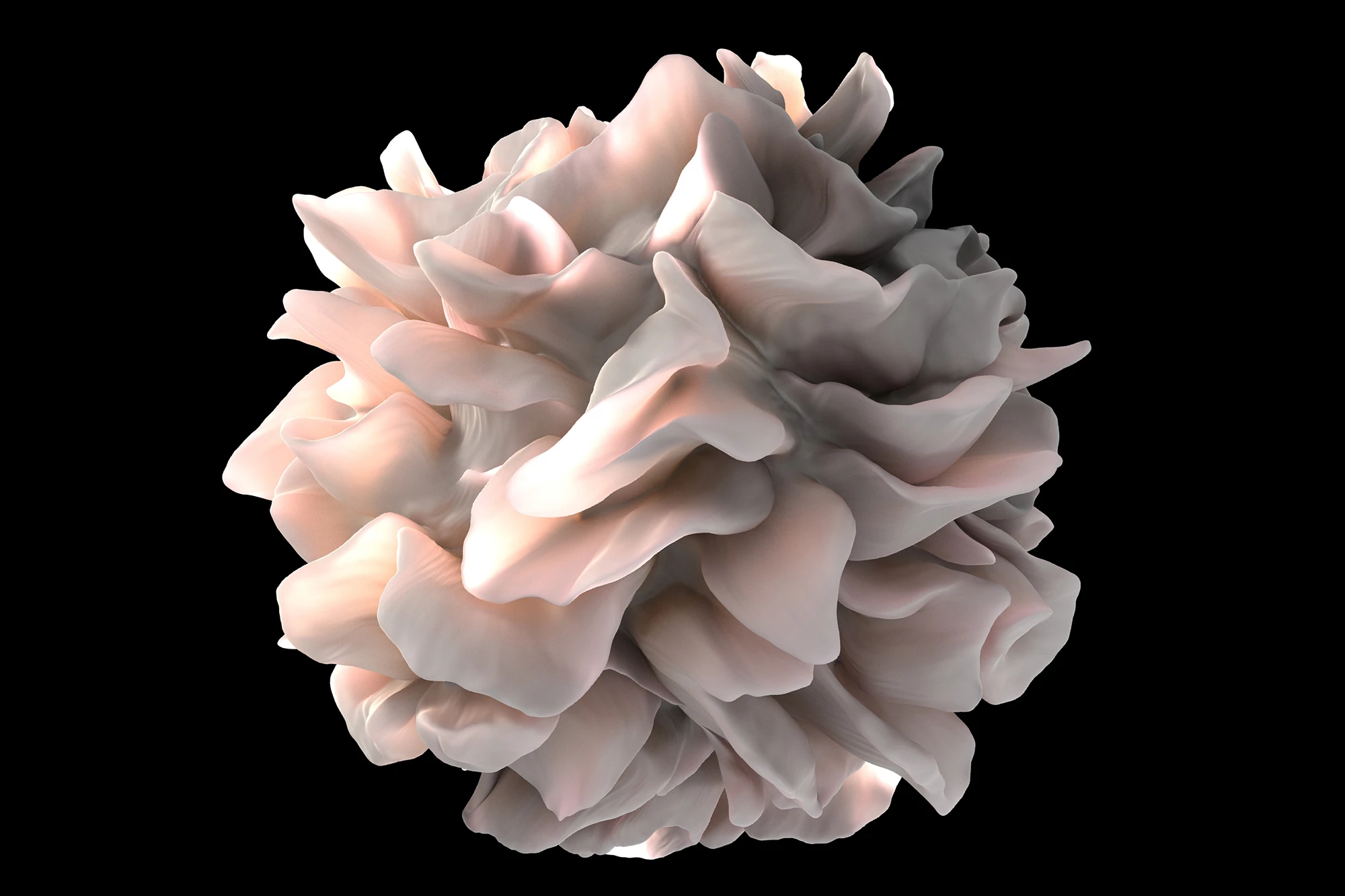
The researchers had previously found that CLNP helped to regulate immune responses and decrease inflammation in autoimmune joint disease. The previous study had shown that CLNP changed the behavior of dendritic cells, specialized immune cells that act as the immune system’s sentinels, initiating and regulating immune responses. In RA, dendritic cells are found in the synovium, the lining of the joints, where they contribute to the chronic inflammation and joint damage that characterizes the disease.
In the present study, the researchers lab-tested Agg-CLNP on human immune cells from healthy people and RA patients and measured changes in inflammatory markers and immune-regulating proteins. They also tested the drug on two different mouse models. The prevention model used a mouse model of RA to see if Agg-CLNP could delay the disease’s onset when combined with an existing RA drug, abatacept (brand name Orencia). The flare model used mice whose arthritis was suppressed with the steroid dexamethasone, then stopped to mimic a flare-up. They tested whether Agg-CLNP, given afterwards, reduced flare severity. For both animal models, the researchers measured joint swelling, ankle thickness, and joint tissue damage under the microscope, analyzed immune cells, and used RNA sequencing to see which genes were turned on or off.
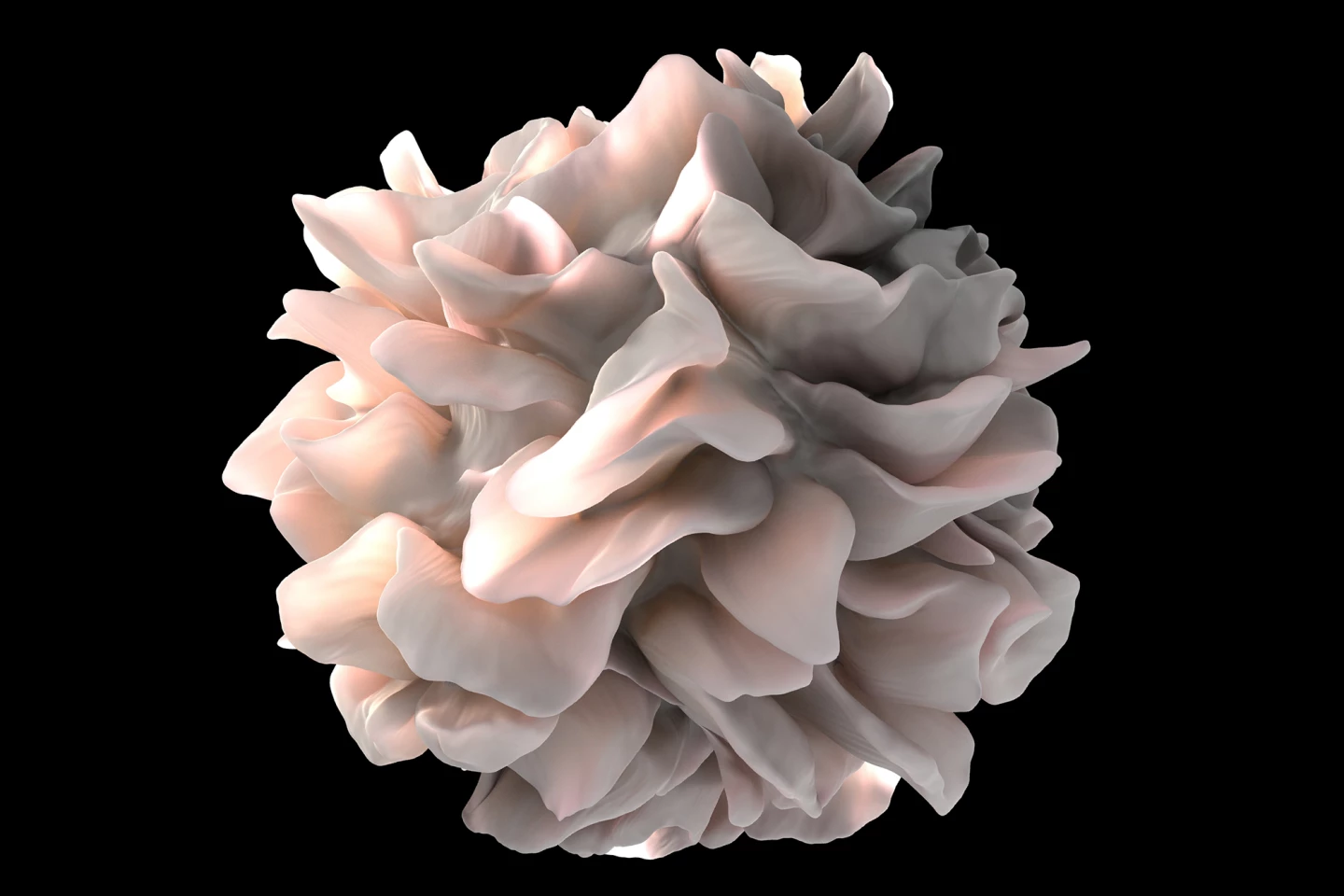
In the human lab cells, Agg-CLNP reduced “go” signals on dendritic cells and increased the “stop” signal linked to dampening immune attacks. In the mouse prevention model, combining Agg-CLNP with abatacept delayed the onset of RA and reduced joint damage more than abatacept alone. The mice had fewer activated T cells and less joint inflammation. In the flare model, when Agg-CLNP was given after dexamethasone, it maintained the immune-calming effect for longer and reduced flare-up severity. Lower levels of pro-inflammatory T helper 17 (TH17) cells were found in the lymph nodes, which drain synovial fluid, and the joints. Gene analysis showed increased expression of anti-inflammatory genes and reduced expression of a pro-inflammatory gene. From a safety perspective, the researchers found that injecting Agg-CLNP locally meant the drug stayed near the joint-draining lymph nodes without changing body-wide vitamin D levels.
The study did have some limitations. It was, of course, preclinical, using in vitro and mouse models; there have been no human trials yet. While mouse models are a good RA mimic, they can’t fully represent the complexity of human RA. Long-term safety, ideal dosing schedules, and the effect of repeat administration of the drug are unknown. And, while gene changes were noted, the exact molecular pathways in humans need to be confirmed.
Nonetheless, if it’s successful in future clinical trials, Agg-CLNP could prevent RA in high-risk individuals, help patients stay flare-free for longer when used with existing treatments like abatacept, reduce steroid dependence, and deliver localized immune-calming signals without suppressing the whole immune system.
The study was published in the journal ACS Central Science.
Source: American Chemical Society via Newswise