Cognitive behavioral therapy (CBT) is a multifaceted approach that’s recommended as a first-line treatment for chronic insomnia. A new study looked at the components of CBT to determine which ones are most effective for improving sleep, finding that relaxation techniques may potentially be counterproductive.
Chronic insomnia can be debilitating, draining a person’s energy and affecting their mood. It can also affect health, with long-term insomnia being linked to an increased risk of high blood pressure, heart attack, obesity, diabetes, depression, and stroke.
Cognitive behavioral therapy for insomnia (CBT-I) uses educational, cognitive, and behavioral strategies to help people get to sleep. Recommended as a first-line, nonpharmacological treatment, it can be delivered in-person or online, through an app or guidebook, with or without a therapist. Previous studies have shown it to be an effective, low-risk option for people with chronic insomnia. However, the effectiveness of each component of CBT-I is unclear.
Researchers from the University of Tokyo Hospital undertook a systematic review and meta-analysis of existing studies to determine which CBT-I components are more effective in treating chronic insomnia and which are less so.
They identified a total of 241 trials, including 31,452 randomized participants with a mean age of just over 45. Participants with psychiatric or physical comorbidities were included, and 67% were women. Treatment duration ranged from one to 16 weeks.
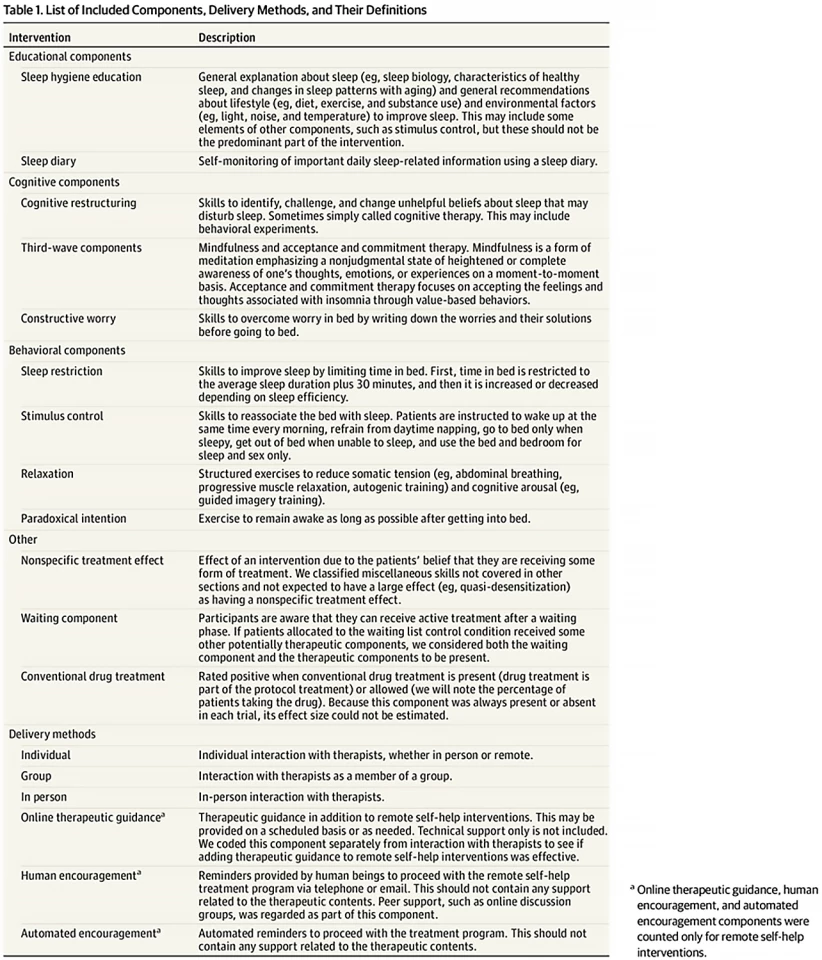
The researchers regarded CBT-I broadly as a psychotherapy that included one or more of the following: cognitive restructuring, constructive worry, third-wave components (mindfulness, acceptance and commitment therapy), sleep restriction, stimulus control, paradoxical intention, and relaxation. They included various delivery formats, including in-person, individual and group formats. Control conditions included waiting list, no treatment, psychoeducation (sleep hygiene education), and treatment as usual. A list of CBT-I components and their definitions appears below.
The researchers analyzed the data using component network meta-analysis (cNMA), an extension of standard NMA that can be used to ‘disentangle’ the associations of different components included in multicomponent interventions with outcomes. They found that cognitive restructuring, third-wave components, sleep restriction, and stimulus control were beneficial for chronic insomnia, while sleep hygiene and keeping a sleep diary did not appear to be essential. Relaxation was found to be potentially detrimental.
The results showed that different components were associated with changes in specific outcomes. Cognitive restructuring and third-wave components helped with sleep quality without significant changes in self-reported sleep continuity (the amount and distribution of sleep versus wakefulness). Sleep restriction was associated with improved ‘wake after sleep onset’ (total minutes awake after first falling asleep) and sleep efficiency (the ratio between the time spent asleep and the total time dedicated to sleep). Stimulus control was associated with improved sleep latency (the time from ‘lights out’ to falling asleep) and sleep efficiency. Regarding delivery format, although following a self-help guide with encouragement from other people was helpful, in-person sessions were found to be more beneficial.
“Overall, our findings identified several essential components of CBT-I which can lead to an intervention that maximizes treatment efficacy, minimizes treatment burden and increases scalability, that is, makes it easier to offer this treatment to more patients,” said Yuki Furukawa, lead author of the study. “Further large-scale trials are needed to confirm these contributions. We hope that our research encourages practitioners who are interested in CBT-I to learn streamlined CBT-I so that, in turn, more people who experience insomnia can be offered this relatively simple, noninvasive, yet potentially powerful psychotherapy.”
The study was published in the journal JAMA Psychiatry.
Source: University of Tokyo






