A decade-long global review has confirmed that good heart health, measured by diet, exercise, and other habits, not only protects against heart disease but also supports nearly every organ system, reducing risks of dementia, cancer, and more.
In 2010, the American Heart Association (AHA) introduced the Life’s Simple 7 (LS7) framework to measure, monitor and modify cardiovascular health (CVH) across the lifespan. The LS7 includes seven metrics: diet, physical activity, smoking status, body mass index (BMI), blood pressure, total cholesterol, and fasting blood glucose.
A new study led by Emory University reviewed global studies conducted in the 10 years since the LS7 was introduced to see how CVH, measured using the framework, affects health outcomes, what determines good CVH, and how it can be improved.
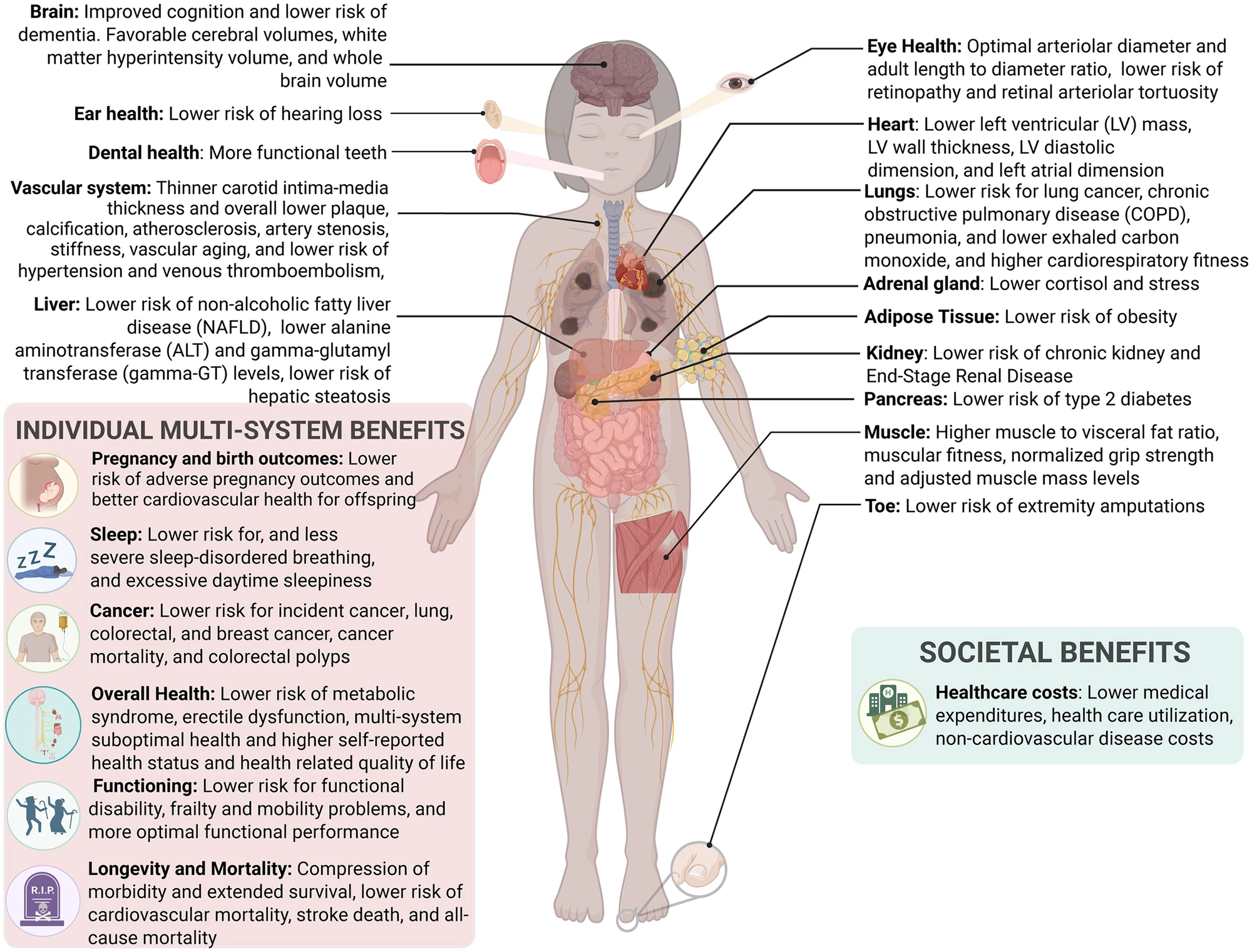
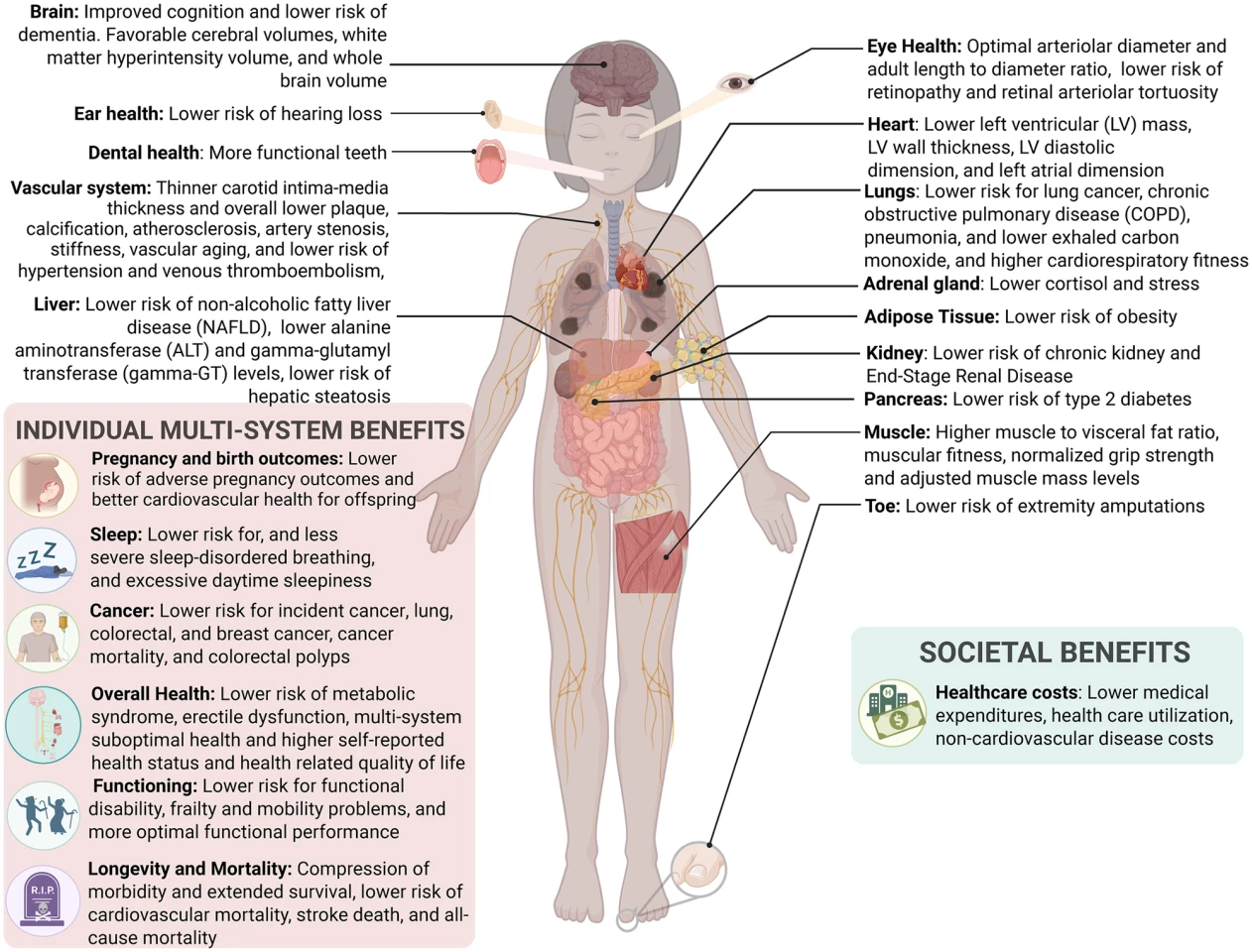
“While we recently learned that heart health and brain health are closely tied, in this review we found that almost every organ system and bodily function from head to toe benefit from a heart-healthy lifestyle,” said lead and corresponding author Liliana Aguayo, PhD, MPH, a research assistant professor at Emory’s School of Nursing and a core member of its Global Diabetes Research Center.
For the LS7, each of the seven metrics is scored on a scale of 0 (poor), 1 (intermediate) or 2 (ideal), and the overall score is the sum of these individual scores, ranging from 0 to 14. Higher scores indicate better CVH. It is worth noting that the LS7 was updated in 2022 to include sleep as a component of cardiovascular health, becoming Life’s Essential 8 (LE8).
The researchers included 483 studies conducted worldwide between January 2010 and January 2021. To be included, studies had to have examined three or more LS7 metrics using health-focused measures. Studies that focused on disease risk scoring tools, non-peer-reviewed papers, reviews and abstracts were excluded. A Mixed Methods Appraisal Tool (MMAT) was used to assess the methodological quality of included studies; most studies were found to have a low risk of bias.
The review found that having high CVH, that is, six to seven “ideal” metrics or a score of 12 or more, was strongly associated with:
- Lower risk of cardiovascular diseases like heart attack, stroke, and peripheral artery disease.
- Lower all-cause mortality.
- Reduced risk of dementia (86% lower), cancer (20%), chronic kidney disease (62%), and depression (a 10% lower risk for each additional ideal CVH metric).
- Better quality of life, lower healthcare costs, and longer lifespan.
A higher CVH was also associated with a lower risk of diabetes, eye health problems, hearing loss, high blood pressure, and high cholesterol. The image below, taken directly from the study, illustrates the researchers' findings regarding the body-wide benefits associated with optimal CVH.
However, there was a low prevalence of ideal CVH. Globally, fewer than 4% of people met all seven ideal metrics. Even when a looser definition (five or more ideal metrics) was implemented, rates remained low. Diet was the least likely metric to be ideal, with less than 1% of people meeting it, while non-smoking was the most common.
All is not lost, though. The researchers observed that even modest improvements, such as improving just one metric, could cut heart disease risk by 20% to 30%. For US adults specifically, improvements from poor CVH to moderate or ideal levels were associated with a 33% lower risk for cardiovascular disease and a 20% lower risk for all-cause mortality.
“Optimal CVH is a powerful predictor of low long-term CVD [cardiovascular disease] risk and future physical and psychological well-being,” said the researchers. “We summarized a large array of multisystem and multilevel benefits associated with ideal/high CVH, spanning from brain to toe.”
The study has some limitations, one of the most significant being the existence of research gaps; there was a lack of data on children, pregnant women, and diverse populations. Also, mechanisms linking CVH to health outcomes are still not fully understood, and the effects of environmental factors such as pollution or chemical endocrine disruptors are underexplored. From a practical perspective, the researchers didn’t preregister their review protocol, thereby raising the risk of publication bias, and only studies using LS7 and not the newer LE8 were examined.
Nonetheless, the study’s findings raise important policy and public health considerations. In clinical practice, clinicians can use LS7/LE8 scores to track and improve patient health, even before symptoms appear. Emphasis should be placed on preventing CVH decline rather than just managing the disease. Even small steps, like improving diet or quitting smoking, can meaningfully reduce long-term health risks. Importantly, the study shows that there’s no need for perfection; modest progress was found to yield real gains.
The study was partly supported by the American Heart Association and the National Institutes of Health. It was published in the Journal of the American Heart Association.
Source: Emory University