Antimicrobial resistance, particularly resistance to antibiotics, is a worldwide problem. A new study has, for the first time, shown how the consumption of antibiotics by an entire population can affect an individual's health.
It’s well-known that the widespread use of antibiotics, antivirals, antifungals, and antiparasitics has led to antimicrobial resistance (AMR). According to the World Health Organization (WHO), AMR is among the top 10 global public health threats. Mis- and overuse of antibiotics, particularly, has contributed to the development of drug-resistant bacteria.
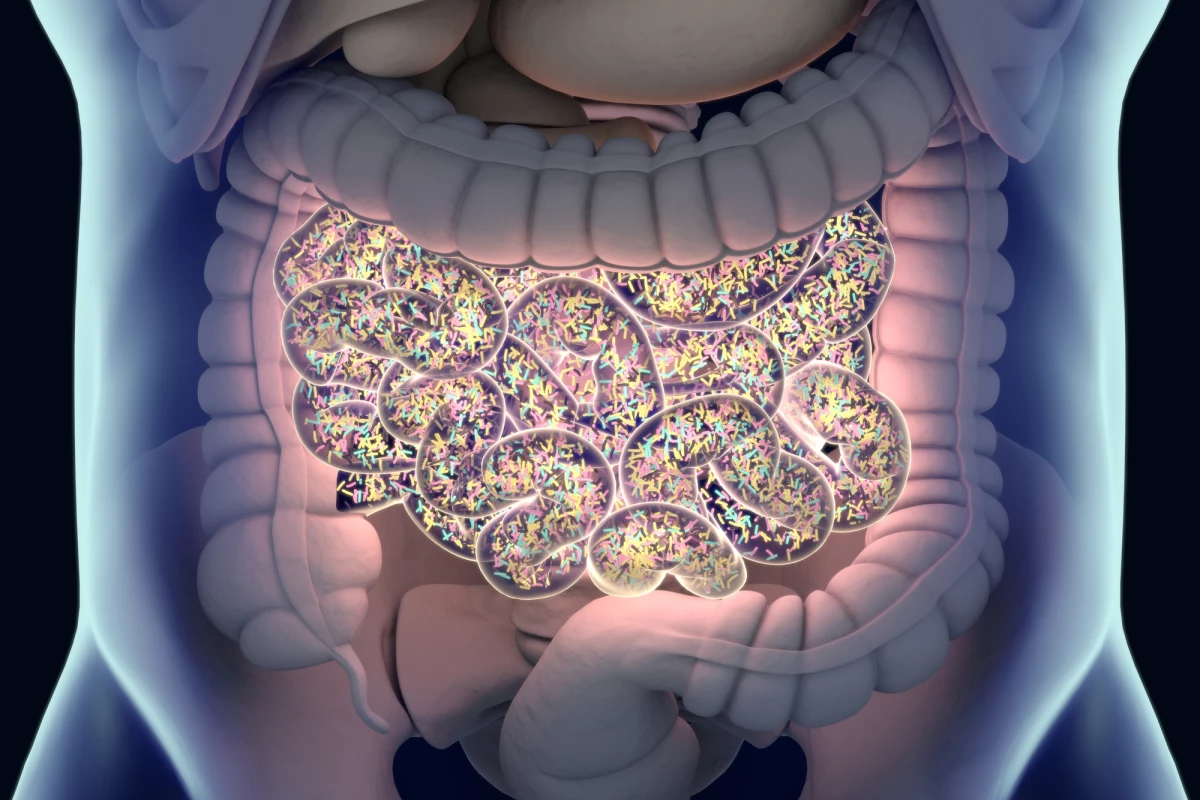
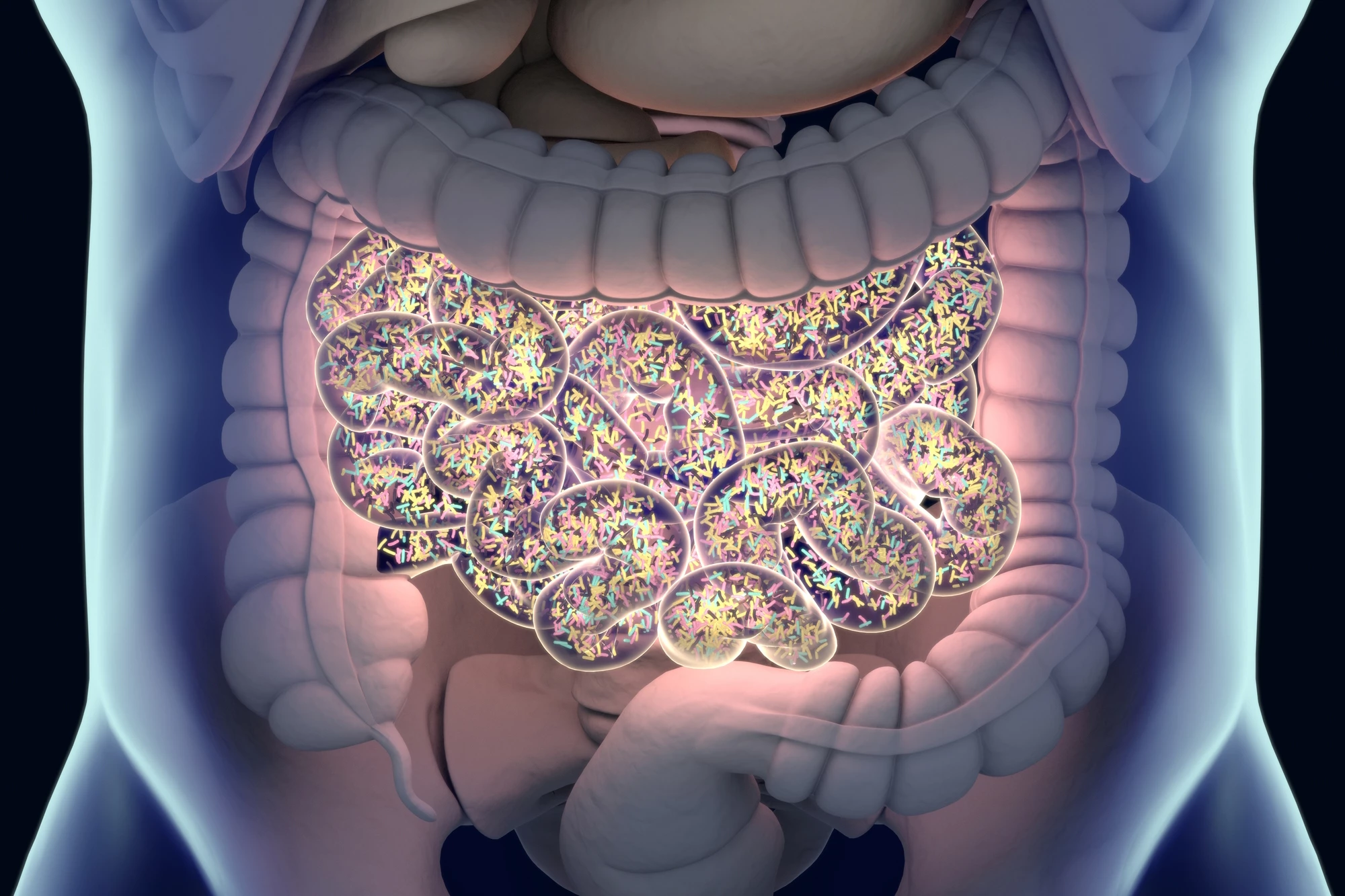
One of the main issues with antibiotics is that in addition to ridding the body of pathogens, they also negatively affect natural flora. The gut microbiome is made up of billions of bacteria and other microorganisms – some helpful, some potentially harmful – that live in the digestive tract. In a healthy person, these microorganisms coexist without issue. But the prolonged use of antibiotics can throw this commensal relationship out of balance, causing the body to be more prone to disease.
There is also a genetic component to AMR. Bacteria of the same or different species share genes with each other through a process called horizontal gene transfer. AMR can result when bacteria pass on antibiotic resistance genes (ARGs), and horizontal gene transfer can occur between strains of bacteria within an individual and in the environment. It can even occur between dead and living cells. Resistance is magnified because bacteria multiply rapidly.
There have been a lot of studies into the short-term impact of antibiotics on the gut microbiome. Still, the consequences on the general population over the long term have not been researched as much.
A new study has examined how a population’s consumption of antibiotics affects the level of ARGs found in that population. Researchers analyzed more than 3,000 gut microbiome samples from healthy individuals across 14 countries.
“Even a healthy individual, who hasn’t taken antibiotics recently, is constantly bombarded by microbes from people or pets they interact with, that can lead to resistance genes becoming embedded in their own microbiota,” said Christopher Quince, corresponding author of the study.
They then compared the ARGs identified in samples to those found in large genome collections to see how the genes moved between microbes and pathogens.
“We deliberately focused on samples from healthy people, or at least those we could be confident weren’t taking antibiotics,” Quince said. “We needed to see the gene profile in the gut microbiome without the influence of any antimicrobials.”
Cataloging the number of ARGs they found, researchers compared their data to the Comprehensive Antibiotic Resistance Database (CARD), a biological database that collects and organizes information on ARGs and their associated phenotypes (observable traits). They identified a median of 16 AMR genes and found that the median number of genes varied across the 14 countries they’d studied.
Using WHO and ResistanceMap data, the researchers demonstrated a strong correlation between the frequency of ARGs in a country and its antibiotic consumption level. ResistanceMap is a web-based collection of data visualization tools for the interactive exploration of AMR and worldwide trends in antibiotic use.
“We found that, in countries where antibiotics are taken more regularly, their populations also have higher numbers of resistance genes in their gut microbiome,” Quince said.
The study’s findings suggest that regardless of a person’s health and whether they’re taking antibiotics, the number of ARGs in the gut is heavily influenced by the population-wide consumption of antibiotics.
“We’ve known for some years that antimicrobial resistance genes can spread incredibly fast between gut bacteria,” said Falk Hildebrand, co-author of the study. “This study is so important because it can, for the first time, quantify the impact national antibiotic usage has on our commensal bacteria, as well as giving us insights into the common types of resistance we can expect to evolve.”
The researchers hope that the insights provided by their study will guide future treatment and the development of new antimicrobial medicines.
The study was published in the journal Nature Communications.
Source: Earlham Institute