Researchers have combined a drug that’s normally used to treat cancer with a naturally derived anti-inflammatory to stimulate pancreatic stem cells to grow into insulin-producing cells. The study’s findings could one day lead to an alternative way of restoring insulin production in people with type 1 diabetes.
In type 1 diabetics, the pancreas’ beta cells are damaged or destroyed by the body’s immune system, producing little or no insulin. Much research has been undertaken to develop treatments to regenerate beta cells, including converting stem cells from elsewhere in the body into insulin-producing cells. According to the International Diabetes Federation, in 2022 there were 8.75 million people in the world living with type 1 diabetes.
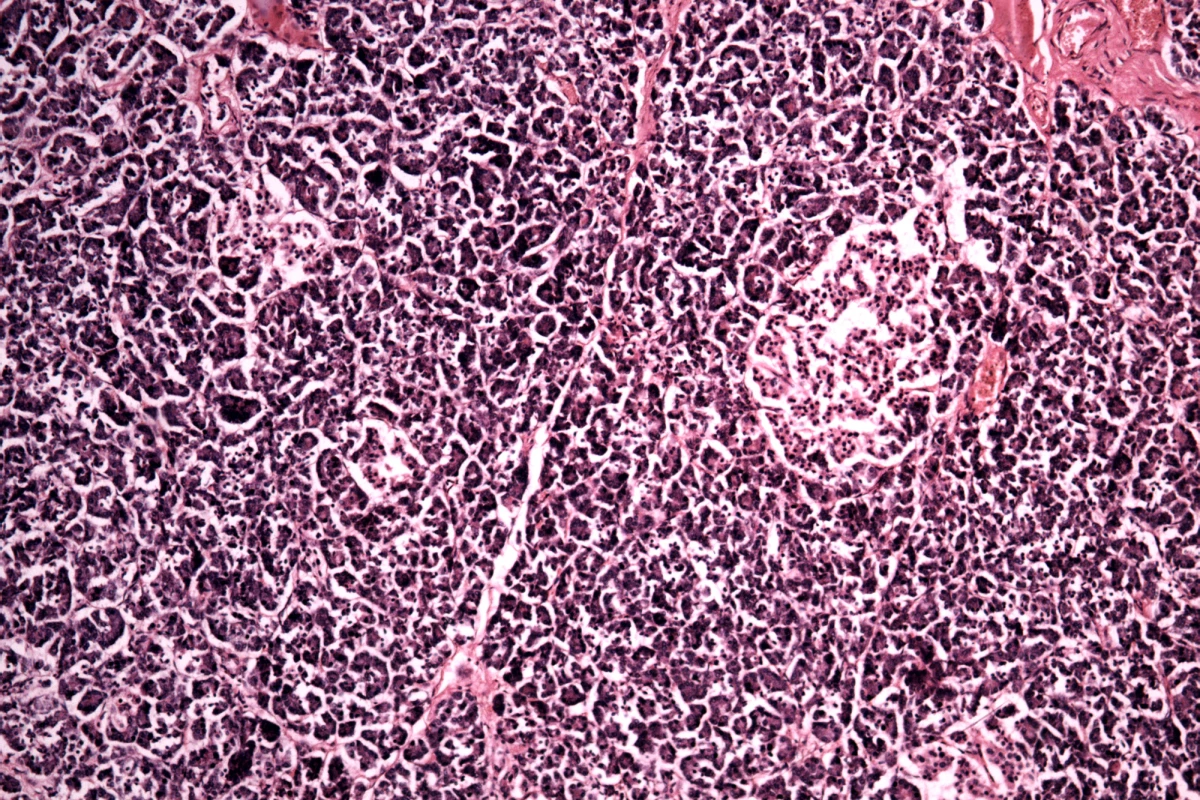
The pancreas consists of exocrine and endocrine cells. Endocrine cells are the ones that secrete hormones, including insulin, and exocrine cells produce enzymes that are secreted into the small intestine and help to digest food. Ductal cells are exocrine cells that form the lining of the tubes (ducts) that deliver pancreatic enzymes. Previous studies have suggested that ductal progenitor cells, descendants of stem cells, can differentiate into insulin-producing beta cells.
Now, in a proof-of-concept study, researchers from the Baker Heart and Diabetes Institute in Australia have used a combination of a synthetic drug and a naturally derived drug to stimulate ductal progenitor cells to differentiate into beta-like cells capable of producing insulin.
The researchers used a synthetic EZH2 inhibitor primarily used for cancer treatment, and triptolide, derived from a Chinese herb and known to have anti-inflammatory and anti-cancer properties. The EZH2 gene provides instructions for making an enzyme that forms part of a protein group called the polycomb repressive complex-2. By turning off particular genes, the complex is involved in determining the type of cell an immature cell will ultimately become. When the EZH2 enzyme becomes overactive, cell growth becomes uncontrolled and can lead to cancer. When used to treat cancer, EZH2 inhibitors target and suppress the enzyme, stopping tumors from developing.
They found that after 48 hours, the EZH2 inhibitor-triptolide combination had restored the progenitor ability of human ductal cells, reactivating them and allowing for their differentiation into beta-like cells. When exposed to glucose solution, the cells produced insulin.
The researchers say that their “experimental observations suggest the possibility that reprogrammed cells were capable of producing insulin and functionally elevated insulin secretion in response to glucose stimulation.”
While further research is needed to examine the mechanism of action of these drugs, the researchers say their study’s findings provide some evidence for a potential alternative treatment for type 1 diabetes.
The study was published in the journal Clinical Epigenetics.
Source: Baker Heart & Diabetes Institute