While the risk of cancer recurrence depends on many factors such as cancer type and how progressed it is, the fear of the disease returning is a serious and long-lasting concern for survivors. Scientists in Japan have come up with a new tool to study the way cancerous cells can hide away in body tissues and spring back into action once the danger appears to have passed, by developing a novel hydrogel that reverts different cancer cell types back to these insidious cancer stem cells.
The trouble with cancer stem cells is that they are resistant to treatments like chemotherapy and radiotherapy, and can stealthily survive in the body and lead to recurrence down the track. Their scarcity means opportunities to study them are limited, so researchers at Hokkaido University and the National Cancer Center Research Institute set out to come up with a way to expand our knowledge of the way that they function.
“Cancer stem cells are a major target for anti-cancer drugs, but they are difficult to identify because they are present in very small numbers in cancer tissues,” explained Professor Shinya Tanaka of Hokkaido University. “Understanding the molecular mechanisms of cancer stem cells is crucial for developing better cancer treatments.”

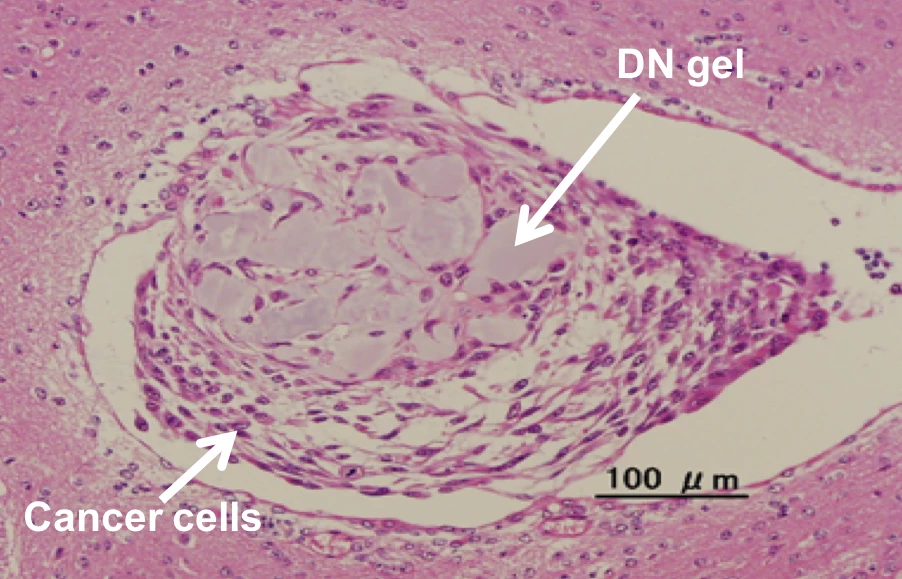
The team's solution is a hydrogel, called a double network (DN) gel, made up of a network of two chemicals and a whole lot of water, which gives it the wet and mushy characteristics of biological tissue. The team placed brain, uterine, lung, colon and bladder cancer cells and sarcoma cells in the gel, all of which responded to the environment by forming spherical structures and producing molecules known to be hallmarks of cancer stem cells, within a 24-hour timeframe.
By observing this process, the team uncovered a few clues about the mechanisms involved in cancer cell reprogramming. Calcium channel receptors and a protein called osteopontin were found to be key to the process, while the brain cancer cells responded by producing what are known as platelet-derived growth factor receptors. This offered the scientists a target, enabling them to introduce a molecular inhibitor of the receptors and effectively eradicate the cancer stem cells.
The hope is that this DN gel can be used to further unravel the secrets behind they way cancer cells are reprogrammed and the way cancer stem cells function, which could lead to more effective drugs to take them out.
“In the future, the DN gel could be used to enhance cancer cell type diagnosis and to produce personalized medicines, which could improve the prognosis of cancer patients,” says Tanaka.
The research was published in the journal Nature Biomedical Engineering, while the video below offers a look at the cells forming spherical structures within the gel.
Source: Hokkaido University