One of the ways scientists hope to lighten the burden of living with type 1 diabetes is through transplantations of cells that produce insulin, shoring up supplies of the vital hormone and safely regulating blood-sugar levels into the future. Rejection of these cells by the host's immune system is a serious stumbling block for this still-experimental therapy, but new bead-like materials offer new hope by neutralizing these attacks and negating the need for long-term immunosuppressant drugs that have severe side effects.
The therapy explored through this research hinges on the transplantation of what are known as beta cells in the pancreas, which are responsible for producing the insulin the body needs to keep blood sugar levels under control. In type 1 diabetes, these cells fall victim to autoimmune attacks which compromises performance of this vital bodily function, creating the need for regular insulin injections for patients to manage the condition.
Harvesting beta cells from a donor pancreas or engineering them through stem cells in the lab before injecting them into patients is a highly promising solution. One key stumbling block in this field of research, however, is the tendency for the patient's immune system to reject the foreign cells, which means those to receive this experimental treatment so far have mostly had to undertake a life-long regime of immunosuppressive drugs to temper immune attacks.
These drugs can have serious side effects, which include an impaired immune system and therefore higher chances of acquiring infections and cancers, along with vomiting, nausea, kidney damage and high cholesterol. So coming up with a way to implant new populations of beta cells without the need for immunosuppressive drugs would mark a major breakthrough, and we are seeing some exciting advances.
As we saw in one breakthrough earlier this year, this might involve deploying novel nanoparticles as vehicles for drug delivery, altering the way they interact with the immune system to dodge serious side effects. Another common approach involves encapsulating the beta cells in carefully engineered materials that protect them from immune attacks without compromising their function.
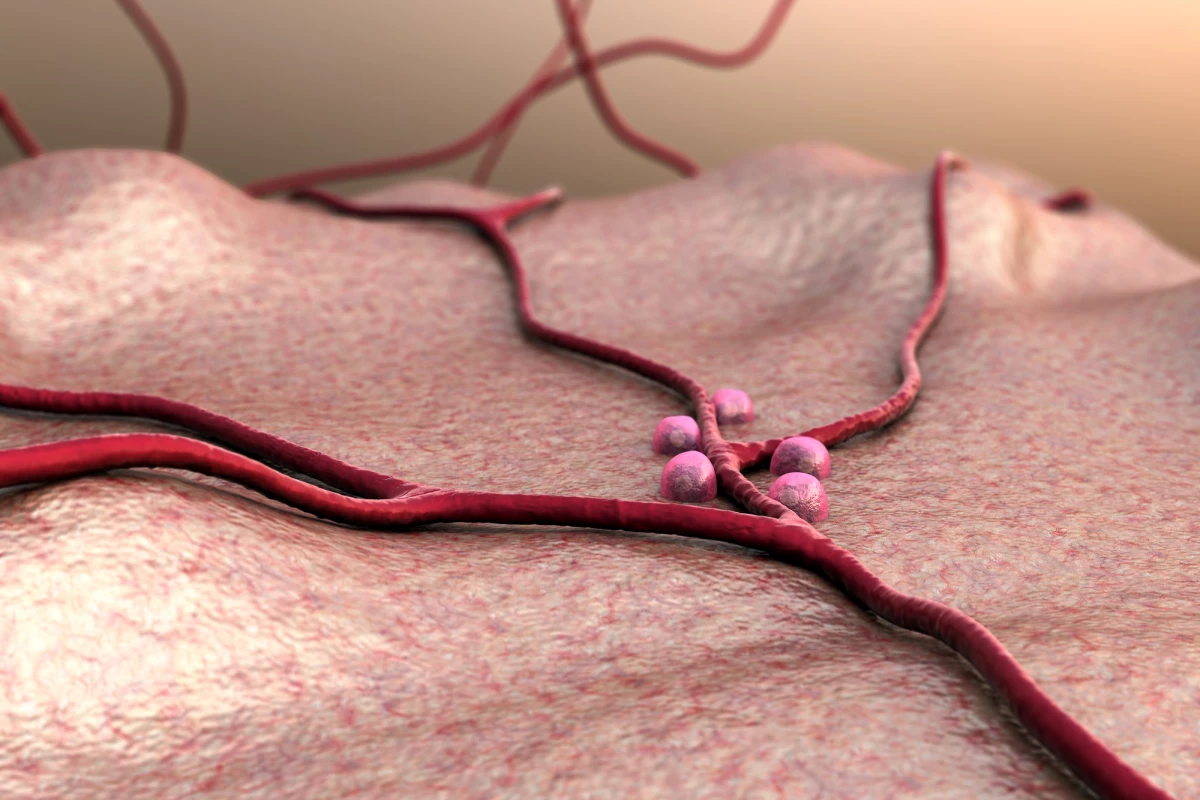
This is the approach being explored by scientists from Massachusetts General Hospital, Harvard Medical School, Georgia Institute of Technology and the University of Missouri. The team has developed a new biomaterial that takes the form of microgel beads bearing a novel protein called SA-FasL on the surface, which promotes immune tolerance. This material was mixed with groups of pancreatic cells called islets, which contain the vital beta cells, and transplanted into a pouch of stomach-adjacent tissue called the omentum, in diabetic mice.
Rather than a lifelong regime of immunosuppressive drugs, the mice received a course of one such drug called rapamycin for three months after the transplantation. The technique ultimately proved very successful, with the cells able to survive and enable the mice to maintain good control of their blood-sugar levels for an extended period.
“Our strategy to create a local immune-privileged environment allowed islets to survive without long-term immunosuppression and achieved robust blood glucose control in all diabetic nonhuman primates during a six-month study period,” says lead author Ji Lei. “We believe that our approach allows the transplants to survive and control diabetes for much longer than six months without anti-rejection drugs because surgical removal of the transplanted tissue at the end of the study resulted in all animals promptly returning to a diabetic state.”
While the therapy is yet to be tested in people, the scientists describe the study as a highly relevant pre-clinical animal model, and hope to use it as a springboard for clinical trials in humans. In addition to showing "great potential" in treating type 1 diabetes, the team also notes there are safety advantages over more common approaches that involve transplanting cells into the liver.
“Unlike the liver, the omentum is a non-vital organ allowing its removal should undesired complications be encountered,” said Lei. “Thus, the omentum is a safer location for transplants to treat diabetes and may be particularly well suited for stem-cell-derived beta cells and bio-engineered cells.”
The research was published in the journal Science Advances.
Source: Massachusetts General Hospital